The spread of CoV-2 occurs mainly by respiratory droplets. Its dispersion depends on several factors: viscoelasticity of fluid, ventilation, evaporation rate, exhalations, sneeze or cough. At moment, the preventive distance to avoid the contamination has been established in 1–2m. We believe that it is necessary to review this aspect, because the respiratory flows change with the intensity of physical activity.
The ventilatory response can be evaluated in terms of ventilatory demand or ventilatory efficiency. During maximal effort tests, athletes mobilize an extraordinary amount of air arriving to 150/200L/min. The respiratory volume follows increase in linear progression during the test in function of power developed. When the air volume is increased 10 times, we think that the distance should be around 6–7m.
Coronavirus disease (COVID-19) is an acute respiratory tract infection that emerged at the end of 2019. It was initiated in China and showed that 13.8% of cases were severe and 6.1% critical. This severe presentation is mainly due to the pulmonary expression of the virus through specific receptors.1
It is believed that CoV-2 (COVID-19) occurs primarily through respiratory droplets, the same way that influenza.2 With droplet transmission, the virus is released into respiratory secretions when an infected person coughs, sneezes, or speaks can infect another person if they come into direct contact with the mucous membranes. Infection can also occur if a person touches a contaminated surface and then touches their eyes, nose, or mouth. The drops generally do not travel more than 2 meters (m) and do not remain in the air. Regarding the period of infectivity, the interval during which an individual with COVID-19 is infectious is uncertain, it seems that SARS-CoV-2 can be transmitted before the development of symptoms and during the course of the disease.2–4 Furthermore, the clinical characteristics of COVID-19 (SARS CoV-2) substantially overlap with influenza and other viral respiratory diseases.5
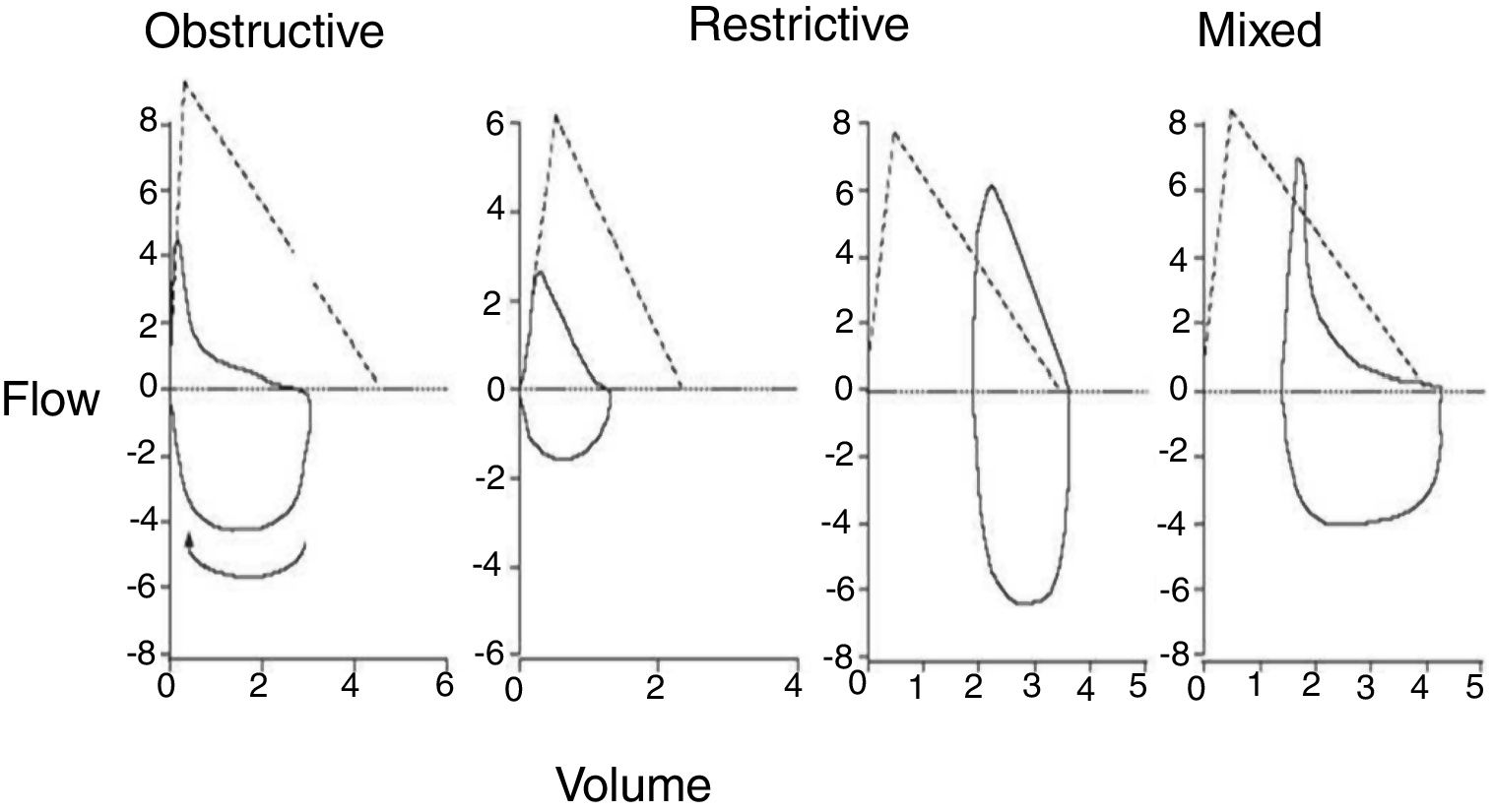
Respiratory flowMeasurements of air flow and lung volume are used to give diagnoses of lung disorders (obstructive and restrictive), to characterize severity, and to control the responses to treatment. The data are reported as absolute flows, volumes and as percentages of expected values.6
In expiratory flow test, is recorded the expired volume: forced vital capacity (FVC) and the expired volume in the first second FEV1). The modern devices measure only the air flow and integrate the time to estimate the expired volume.6,7
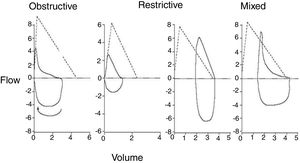
Spirometry and volume flow curveThe forced spirometry includes FEV1 and FVC measurements as indicators of airway status.6,8 The morphology of the flow volume curve is useful for detecting the characteristic the slowdown of expiration at low volumes in obstructive problems and the convexity of curve in restrictive cases. When the FEV1/VC ratio is less of 70% it is compatible with an obstruction problem6–10 (Fig. 1).
In general, in healthy subjects, respiratory function is not usually decisive or limiting the performance in aerobic endurance sports.11 Training programs that include exercising leg muscles as running or cycling are commonly used both in sedentary populations as well in patients with diverse pathology (chronic obstructive pulmonary disease, chronic heart failure, arterial hypertension, etc.) to improve their performance, reduce perception of symptoms and improve the quality of life.12
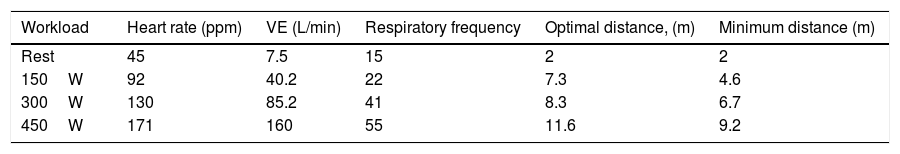
The ventilatory response to exercise can be evaluated in terms of ventilatory demand, ventilatory efficiency and profile of respiration. Ventilatory demand [total ventilation (VE)], can be assessed as the relative contribution of tidal volume (VT) and respiratory rate (RR). The efficiency ventilatory (VE) must increase with the production of carbon dioxide (VCO2) (that is, the slope and the VE/VCO2 ratio).12–14
Ventilation per minute (VE) is about 5–6L/min at rest
[VT=0.5L−0.1 (dead space)×RF=12–15breaths/min)
In sedentary people, the maximum respiratory rate (RRmax) reaches 35–45breaths/min, however, in elite athletes it reaches 60–70breaths/min. Also, the maximum tidal volume (VTmax) can reach about 2–2.5L (VT does not usually exceed 55–65% of the VC, both in sedentary and athletes).15,16
Modifications in VT and RF have influence in alveolar ventilation (VA). This (VA) is the amount of air that go into the alveoli every minute and participates in the respiratory exchange. This fact is fundamental because this respiratory exchange only occurs in the alveoli and not in the respiratory tract (airways). Di Paco et al.17 have demonstrated that an improved ventilatory profile response after training, must contributes to increased sports performance, despite the fact there are no significant changes in heart rate (HR) at a determinate rate.
The organism is continually undergoing changing O2 demands, that depend on metabolic activity, therefore, ventilation must adapt to this demand by increasing the respiration rhythm and carrying out a more appropriate respiration.18 Professional and/or recreational athletes respire with greater ventilatory volumes of air and a lower respiratory rate. This fact is due to the constant stimulation of respiratory center and the training of respiratory muscles. Higher thoracopulmonary elasticity improves ventilatory mechanics and alveolar ventilation.15,16,18
Since the respiratory flow are high when are increased the metabolic needs and the physical requirement are increased, this high volume of mobilized air can determine the behavior and the safety measures that should be taken when doing exercise in these circumstances of possible contagion by COVID-19.
What should be the safety distance? RecommendationsTransmission of COVID-19 is not well characterized, but it is likely to be like SARS, spreading by droplets and the air.19 Also, coronaviruses can persist on inanimate surfaces (metal, glass or plastic) for at least 9 days, and can be inactivated with an efficient disinfection procedures.20
The dispersion of the drops depends on several factors: viscoelasticity of fluid, exhalation, type of ventilation, expiration rate, evaporation rate and turbulent cloud of drops generated during exhalations, sneezes or coughs.21 Thus, understanding evaporation and dispersion of droplets is important for developing an effective control method for infectious diseases, because the distance to which the drops can move is related with the distance at which is possible contaminate and transmit the diseases.21
Therefore, it is appropriate to review the infection control rule established in 1–2m3. Now, most horizontal droplet transmission studies show distances of more than 2m. Bahl et al.22 in their review indicated that there are few studies on horizontal spread of droplets in medical journals. By this, they have reviewed in other sciences such mathematical and engineering disciplines to emit they conclusions. They have concluded that the maximum distance in 8m. On the other hand, Cui et al.,23 have indicated that the contamination makes the coronavirus more lethal.
As have indicate Morawska and Cao,24 it is extremely important to recognize the reality that the virus spreads through the air. Also, adequate control measures should be implemented to prevent further spread of the disease by droplets with SARS-CoV-2 through the ventilation system.
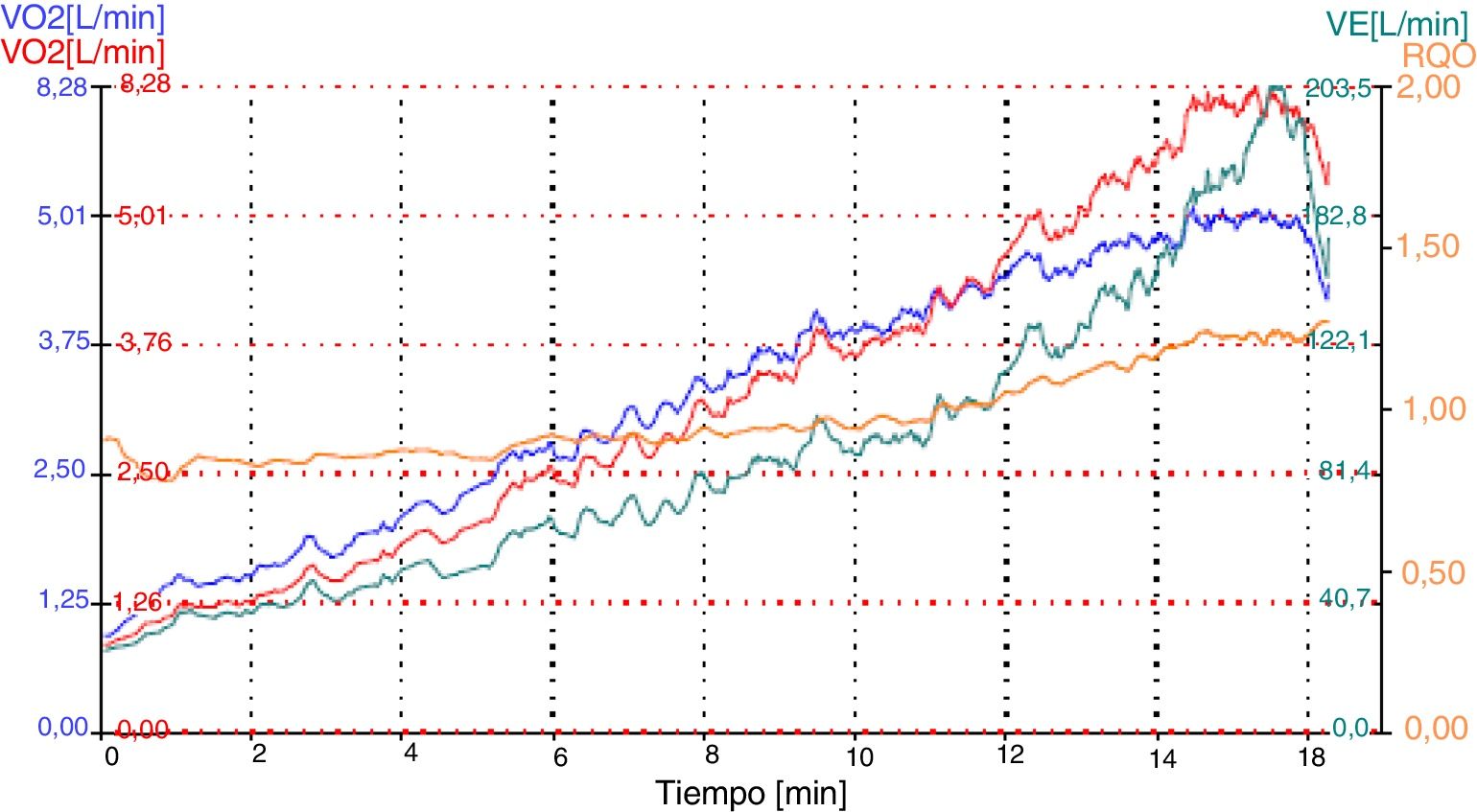
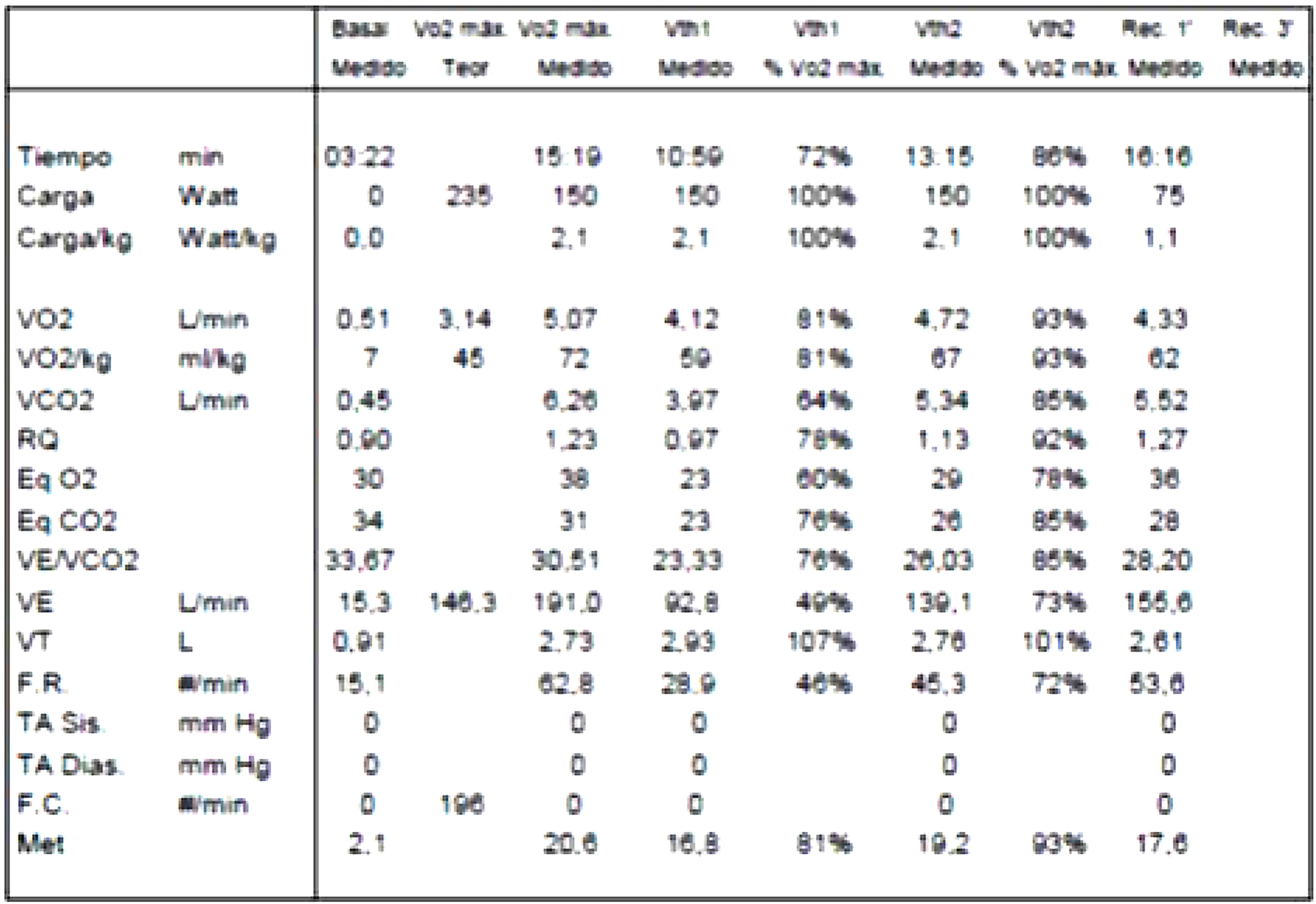
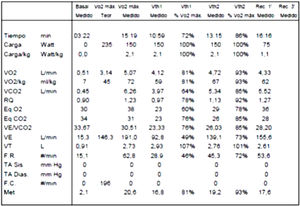
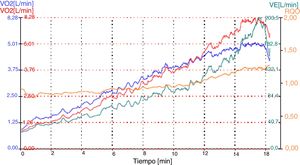
Problems of respiratory: volumes and flows in athletesFrom the data collected in the numerous stress tests, with ergospirometer that we have carried out over the years, we have observed how the respiratory volumes vary throughout the test in athletes. In a maximum incremental test from 1min per step starting at 125W and ending between 350–400W (maximum), the athlete moves about 20–30L/min and at the end of maximal test they end up mobilizing volumes between 150/200L/min. Correspondingly, the respiratory volume increases quite linearly throughout the test (Table 1) (Fig. 2).
In the figure we can observe that the respiratory flows are very important from the beginning. That knowledge determines the safety distance, which helps to avoid contamination among athletes. As shown in the figure, as we increase the power (W), the ventilation (VE) increases, too. In a mathematical model we can establish that the radius of reach (distance) increases with the square root of the increase in power made during the effort. Therefore, and considering these data, when the air volume is increased by 10 times, the distance (m) should be multiplied by approximately 3, and we would go from 2m to 6–7m away. Remember that 2m is the recommended distance for normal subjects.3
On the other hand, if we analyze the dispersion based on the launch of particles, that is, the “parabolic shot” of the same, the flow also depends on the exit velocity. That is, although we have 10 times greater volume, the respiration frequency also increases, so the exit speed is not 10 times more. In general, the respiratory rate practically doubles at the end of the test, therefore, the exit speed will be 5 times greater. In this case, the reach distance in the worst case would be multiplied by 5, going from 2 to 10m.
Safety distanceFor as, is clear that we should increase the safety distance in proportion to the intensity of the athlete's workload. We consider a linear increase in the safety distance with to the respiratory flow (VE), which would guarantee the optimal distance (Table 2). However, we made the distance calculation with real data, by this we will be more cautious with the recommended distance. It is important for us to consider an increase in distance based on the square root of the increase in respiratory volume (Table 2).
Leuven and Eindhoven,25 though by different methods, have indicated that the rule of social distancing (1–2m) seems effective when standing, but when people go for a walk, run or ride a bicycle, caution must be increased. These authors inform that for example during a race (competition) someone breathes, sneezes or coughs, these particles remain in the air and therefore the person running behind passes through this cloud of droplets.
The study of Leuven and Eindhoven25 was carried out by simulating the appearance of saliva particles from people during movement (walking and running) and from different positions. They have concluded that when COVID-19 is considered, the recommendation is to stay out of the stream of droplet dispersion, what we call it the “spray.” Likewise, they indicate that the risk of contamination is greater when people go one after the other. They conclude that people moving in the same direction in one line should keep at least 4–5m distance, and for running and ride in bicycle slow it should be 10m and for cycling at high intensity, it should be at least 20m. Also, when passing (advance) someone, it is recommended to be in a different lane and in a considerable distance away.
The difference between the work of Leuven and Eindhoven25 and ours is that they have carried it out by simulation in a special room and our research is based on respiratory flows with real data during an incremental test to maximum. However, both have come to similar conclusions.
ConclusionsHealth authorities3 are giving guidelines about the safety distance that people must maintain in order to avoid contagions. These guidelines are made for sedentary people, who do not practice physical activity in general. The problem is in athletes, in whom increase their respiratory flow (quantity and frequency) and thus the distances should be greater. As we have indicated before, in the sports field we must adapt the distance to metabolic requirements, demand more meters, around 10m when we perform a maximum stress test.
It seems that in Spain, both the Higher Sports Council (CSD) and the Federation of Sports Facilities Entrepreneurs (FNEID) are preparing a proposal to open sports centers and gyms after COVID-19 indicating safety distances (made randomly). That is why, as the safety distance cannot be controlled in confined space, athletes should wear suitable masks to avoid the transmission of particles.
Therefore, as results from our study and the considerations made by the Belgian/Holand group, we believe that the assessment of the secure distance must be more accurate precise specially when we want practice physical activity. Without any doubt we think that is very important to mind the respiratory flows.
Conflict of interestThe authors declare that they don’t have any conflict of interests.
We thank Ms. Lydia LESHCHANKA, Gomel State University in Belarus, for her help in translation the text into English.