Las lesiones agudas de isquiotibiales son las más frecuentes en el fútbol profesional, y la porción larga del bíceps (LHBF) es el músculo más afectado, siendo las localizaciones proximales las más habituales y con importantes características clínicas, como el tiempo de baja y el riesgo de recaída. Se presentan dos casos clínicos de lesiones proximales de la LHBF: una lesión miotendinosa típica y una menos frecuente que afecta el tendón libre de la LHBF. Las lesiones de la unión miotendinosa localizadas en los isquiotibiales pueden tratarse de manera conservadora, aunque en futbolistas profesionales, donde la cantidad de tejido conectivo afectado es grande (tendón libre), las lesiones deben ser tratadas quirúrgicamente.
Acute hamstring injury is the most common muscle damage in professional footballers and long head biceps femoris (LHBF) is the most commonly affected muscle with proximal locations being most prevalent with important clinical features such as time of recovery and risk of re-injury. Two clinical reports of proximal LHBF injuries are presented: a typical miotendinosus junction (MTJ) injury and a less common injury affecting the free-tendon of LHBF. MTJ injuries located in hamstrings can be treated conservatively but in professional football players, when the amount of connective tissue involved is great (free-tendon) injuries have to be treated surgically.
Introduction
Acute hamstring injury is the most common muscle damage in professional footballers representing around 12% of all injuries.1,2 Long head biceps femoris (LHBF) is the most commonly affected muscle with proximal locations being most prevalent with important clinical features such as time of recovery and risk of re-injury.3 In addition, even though of the implementation of preventive exercises and measures for reducing the incidence, training-related hamstring injuries increase 4% annually and around 1.5% match-related injuries in men’s professional football.4 Magnetic resonance imaging (MRI) exams with a field strength of at least 1.5T and T2 weighted sequences with fat-saturated and/or short tau inversion recovery (STIR) sequences can be helpful in verifying the diagnosis and to prognosticate lay-off time.5
Two clinical reports of proximal LHBF injuries are presented: a typical miotendinosus junction (MTJ) injury and a less common injury affecting the free-tendon of LHBF. A comparison between clinical aspects, MRI characteristics and differences in management are exposed in the discussion.
Case reports
Case 1
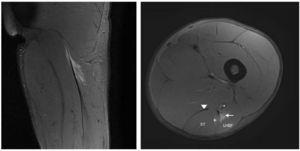
Nineteen years old professional football player suffered sudden pain in his posterior, upper part, thigh when sprinting and was unable to play. Clinical signs showed an acute ham-string strain (painful palpation, limited range of motion (ROM), decrease of strength, painful stretching and difficulty to walk normally). MRI was performed 24 h post-trauma with a 3-T scanner (Titan Vantage, Toshiba). LHBF injury and its characteristics are described in Figs. 1 and 2. The final diagnosis was a proximal MTJ injury of LHBF localized at 10 cm from the ischial tuberosity and 6 cm from the onset of the MTJ. The expected lay-off time was 7-8 weeks. The recovery treatment consisted basically in 3 stages: physiotherapy measures, strength and neuromuscular training in the gym and specific individual football training in the field.
Figure 1 Coronal and axial T2 Fat-saturated images of the left hamstring showing focal partial tear (fiber disruption) in the proximal MTJ of LHBF represented by an area of high signal intensity adjacent to the MTJ (arrow). Note also few disrupted muscle fibers in semitendinous (+). Semitendinosus muscle belly (ST), proximal long head of biceps femoris (LHBF), semimembranosus tendon (arrowhead) and sciatic nerve (*). Feathery pattern of muscle edema can be seen in coronal view.
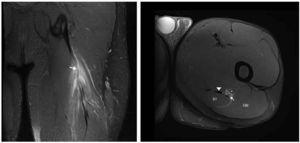
Figure 2 Coronal and axial T2 Fat-saturated images of the left hamstring show thickening and signal intensity changes of the free tendon (arrow), blurring contours and discontinuity that extent until proximal MTJ. There is mild distal retraction of the proximal MTJ. Semitendinosus muscle belly (ST), gluteus maximus (GM), semimembranosus tendon (arrowhead) and sciatic nerve (*).
Case 2
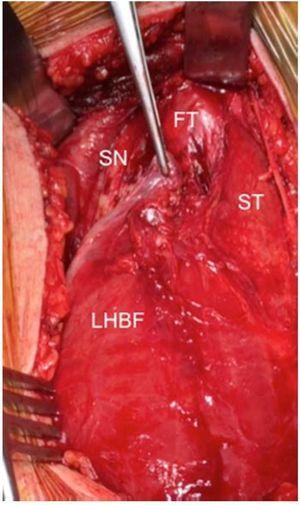
Eighteen years old professional football player suffered the same kind of pain in the same kind of circumstances. Clinical signs were exactly similar than the previous acute hamstring strain described but the MRI exam showed different images (Figs. 3 and 4) because the injury was located in the free tendon of BF. The length of free-tendon was 8.5 cm and the injury was located at 6.5 cm from the ischial tuberosity. Due to the long time of recovery and a high reinjury rate, surgical treatment should be considered. Excision of the scar tissue, including the torn portion of the tendon was then performed and tension-free suturing of the belly remnant of the biceps femoris to the adjacent semitendinosus. In order to provide tension to the tendon and reinforcement with anchors in ischial tuberosity (Figs. 3 and 4).
Figure 3 Intraoperative view. Free-tendon (FT), sciatic nerve (SN), semitendinosus (ST) and LHBF (long head of biceps femoris).
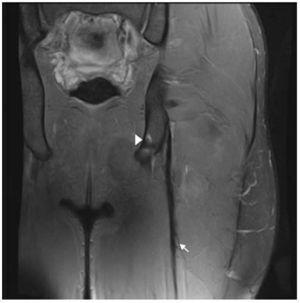
Figure 4 Coronal T2 Fat-saturated image of left hamstring in post surgery follow-up, that show the metallic anchor in ischial tuberosity (arrowhead) and peritendinous sutures represented by magnetic susceptibility peritendinous artifacts (arrow).
Discussion
Hamstings injuries located in MTJ proximal are the most frequent injuries in football players.3 In both presented cases the injured muscle, the mechanism of the injury, initial symptomatology as well as physical examination were the same. However in the second case the majority of the affected connective tissue was mainly tendinous and the symptoms disappeared in several days because of the poor vascularization and innervation of the tendon.
The incorporation of 3T MRI units allows us to visualize smaller tendinous injuries than other methods could have done it. For example tiny ‘‘split’’ longitudinal and transversal lesions, that causes a loss of tension and muscle belly retraction.6
Complete tendon healing is slower, difficult and very low quality. So muscle healing and the presence of disruption of the tendon fibers would be associated with far longer recovery times and a high risk of reinjuries.7 In this situation non-operative treatment results in reduced patient satisfaction, with significantly lower rates of return to pre-injury level of sport and reduced hamstring muscle strength.8
Hence surgical reconstruction in professional players should be the gold standard in spite of the fact that the symptoms disappear quickly and the player did not accept this suggestion that surgery is the appropriate treatment. Surgery should be performed within the first two weeks after the injury9 because of acute surgical repair had significantly improve patient satisfaction, pain relief, strength/endurance, and higher rate of return to pre-injury level of sport. Later repair is associated with higher risk and major complications and re-injuries.8,10
For recreational sport patients, later repair or reconstruction might be considered with an expected 87% return to normal activities for daily living. In case of professional players who need to return to the same level of competition acute repair is strongly recommended.11,12
We recommend an elastic bandage for one to two weeks post- operatively without immobilization, casts, or orthoses. Postoperatively for two to four weeks, hip flexion together with knee extension only allowed. Light touch weight-bearing is permitted with gradual progression to full weight-bearing at the end of six weeks. After three to four weeks, light pool training including swimming is introduced, and after four to six weeks cycling is included. Range of motion hamstrings exercises start during this phase, but stretching exercises should be avoided during the first four weeks. Progressing to running and more active muscle training is advised two to four months after the operation depending on the patient’s progress. The expected lay-off time in this case is 4-5 months.
In summary those injuries that affect free-tendon or most of the MTJ (longer free-tendon more than shorter free-tendon) require surgery. Otherwise for those injuries that affect the MTJ away from the tendon with a small part of connective tissue involved the conservative treatment has to be considered as a first option.
Received 12 April 2017;
accepted 2 May 2017
Available online 31 May 2017
∗ Corresponding author.
E-mail address: xavier.yanguas@fcbarcelona.cat (J. Yanguas).