Anterior cruciate ligament (ACL) tear is a serious and debilitating injury with significant physical, psychological, and socioeconomic consequences. Perturbation-based balance training (PBBT) is a type of neuromuscular training that involves the manipulation of mobile support surfaces, using controlled, unpredictable, multidirectional forces, in order to perturb the balance of the trained individual and thus improve the efficiency of muscle contraction patterns and the dynamic stability of the lower extremity joints. The aim of this review is to analyze the efficacy of the PBBT as a neuromuscular re-education method of choice for the recovery of functional capacity in individuals with ACL knee rupture. A systematic search was carried out in PubMed, Cinahl, Cochrane Library, Medline, PEDro Physiotherapy Evidence Database, Scopus, Web of Science and Sport Discus during January 2022. Only randomized clinical trials conducted in humans and published in English or Spanish were considered. The methodological quality was assessed using the PEDro scale and the risk of bias using the Risk-of-Bias tool of The Cochrane.12 studies were included. In 3 of them, the intervention with PBBT took place before ACL reconstruction, in 7 after ACL reconstruction and in 2 the subjects did not undergo surgical intervention. PBBT appears to be effective in the non-surgical recovery, improving joint stability and neuromuscular control. It was also effective as a preoperative treatment in normalizing knee excursion after ACL surgery. In contrast, the evidence does not support its efficacy as the neuromuscular re-education method of choice in the return-to-sport phase in previously operated athletes.
Knee joint injuries are among the most common injuries in sports-type activities and account for 10–25% of all injuries. Among them, those specifically affecting the anterior cruciate ligament (ACL) account for 45% of the total.1 Some studies put their annual incidence at 68.6 cases per 100,000 person-years, making ACL rupture a common orthopedic injury.2
The ACL is a very important primary structure in the stabilization and biomechanics of the knee, whose main function is to prevent anterior displacement of the tibia in relation to the femur and, to a lesser extent, to control laxity in valgus, varus and rotation during loading on the lower limb. However, the ACL, in addition to being a mechanical restraint, is also a somatosensory organ thanks to the mechanoreceptors that are housed in it and provide sensory feedback to the neuromuscular system, thus contributing to the functional stability of the knee joint.3
ACL tear is a severe and debilitating injury with significant physical, psychological and socioeconomic consequences in both the short and long term, with an elevated risk of developing early osteoarthritis as a major concern.4 Studies quantify this risk in up to 13% of patients with isolated ACL injuries and up to 48% of patients with combined injuries at 10-year follow-up after ACL injury or reconstruction.5
Approximately 70% of cases, the mechanism causing the ACL injury is a non-contact mechanism usually occurring during physical activities requiring deceleration and acceleration, change of direction, landing and pivoting manoeuvres.1 The remaining 30% is due to direct contact with another person or object in which the leg is pinned to the ground and receives sufficient external forces to cause the ligament to tear.6
It should be noted that there is a higher incidence of rupture in women than in men, mainly due to the increased Q-angle, decreased intercondylar space and muscle response, which, in turn, is determined by strength, stiffness and hormonal influence.7 Statistics from the National Collegiate Athletic Association show that in activities involving men and women, with similar rules and equipment (e.g. football, basketball, and volleyball), women are eight times more likely to sustain an ACL injury than men.8
The scientific evidence supports the surgical option as the treatment of choice for individuals who want to return to high-level physical activity after an ACL tear.9 It is also the preferred option for so-called "non-copers", i.e. individuals who have such joint instability that they are unable to continue their previous activities, regardless of their level of demand, and who account for 60% of cases.10 However, there are circumstances in which people try to regain their previous lifestyle without undergoing surgery and choose the conservative therapeutic option, based on physiotherapy. This is the case of the so-called "copers", individuals with knee instability that does not prevent them from continuing with their previous life, but it is also the case of athletes who, due to their life or sporting situation, choose to delay surgery, at least in the short term.10
Neuromuscular training aims to resolve many of these deficits and restore the dynamic stability of the joint. Together with strength training, it is a prevalent method in the rehabilitation and prevention of knee injuries.11
One type of neuromuscular training is perturbation-based balance training (PBBT), or the manipulation of moving support surfaces, using controlled, unpredictable, multidirectional forces to perturb the trainee's balance and improve the effectiveness of muscle contraction patterns and the dynamic stability of the lower extremity joints. Forces could be applied in a static position, in support on one or both feet, or during gait, and through a variety of means ranging from the more complex, such as the Balance Master, to the simpler, such as balance boards (Freeman and Bohler plates) or boards with wheels. In essence, the PBBT is an advanced form of balance training.12,13
Previous reviews addressed the study of PBBT, but not exclusively or systematically. Thus, in 2010, Pezzullo et al.14 published a literature review, which discusses different areas in rehabilitation after ACL injuries, including PBBT. However, this is a non-systematic review, which also includes non-randomised trials.
More recently, Carter et al.15 conducted a systematic review analysing the effectiveness of three preoperative rehabilitation programmes, including a study on PBBT. However, the other trials focus on various aspects of rehabilitation such as muscle strengthening, motor control and balance.
Given the lack of scientific evidence, we propose this review with the aim of analysing the efficacy of PBBT as the neuromuscular re-education method of choice for the recovery of functional capacity in individuals with ACL knee rupture.
MethodsA systematic search of eight electronic databases: PubMed, Cinahl, Cochrane Library, Medline, PEDro Physiotherapy Evidence Database, Scopus, Web of Science and Sport Discus was carried out during the second half of January 2022.
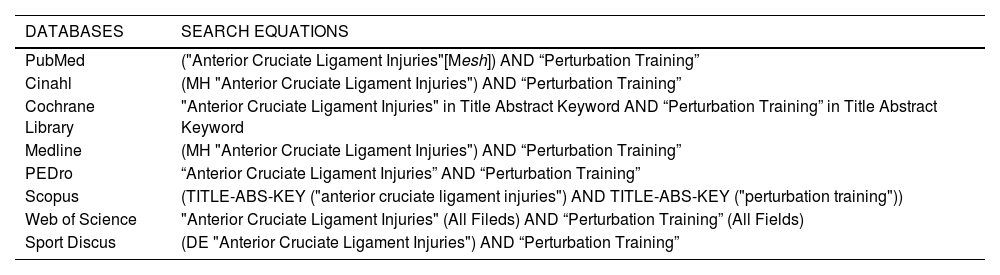
The descriptors used were the Medical Subject Heading (MeSH) term "Anterior Cruciate Ligament Injuries" linked by "AND" to the key term "Perturbation Training". Table 1 shows the equations used for each of the databases consulted. No automatic filter was applied at the time of launching the searches.
Databases and search equations.
MH:Medical Heading; Mesh:Medical Subject Heading; TITLE-ABS-KEY:Title-Abstract-Keyword; DE:Descriptor.
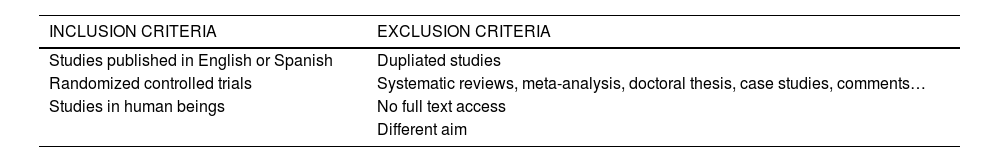
With the results obtained in this first stage, and once duplicate records had been eliminated, a manual screening was carried out according to the inclusion and exclusion criteria specified in Table 2.
Apart from the identification of records through the databases, and once the screening and inclusion phase was completed, a manual search of the citations of the studies selected for inclusion in the systematic review was performed.
The methodological quality of all included studies was assessed based on the criteria of the PEDro scale, a scale consisting of 11 criteria that help to quickly assess which RCTs have external validity or applicability (criterion 1), sufficient internal validity (criteria 2 to 9) and sufficient statistical information to make their results interpretable (criteria 10 and 11).16,17
On the other hand, the risk of bias was assessed for each study using the Risk-of-Bias tool, in its second version (RoB 2), with the aim of documenting the possible flaws and limitations of the RCTs selected in the review. RoB 2 assesses bias in five different domains. Within each domain, one or more key questions are asked and, depending on the answers obtained, three levels of judgement are established: "low risk", "some concerns" or "high risk". Finally, the judgements made for each domain lead to an overall judgement for the study being assessed.18
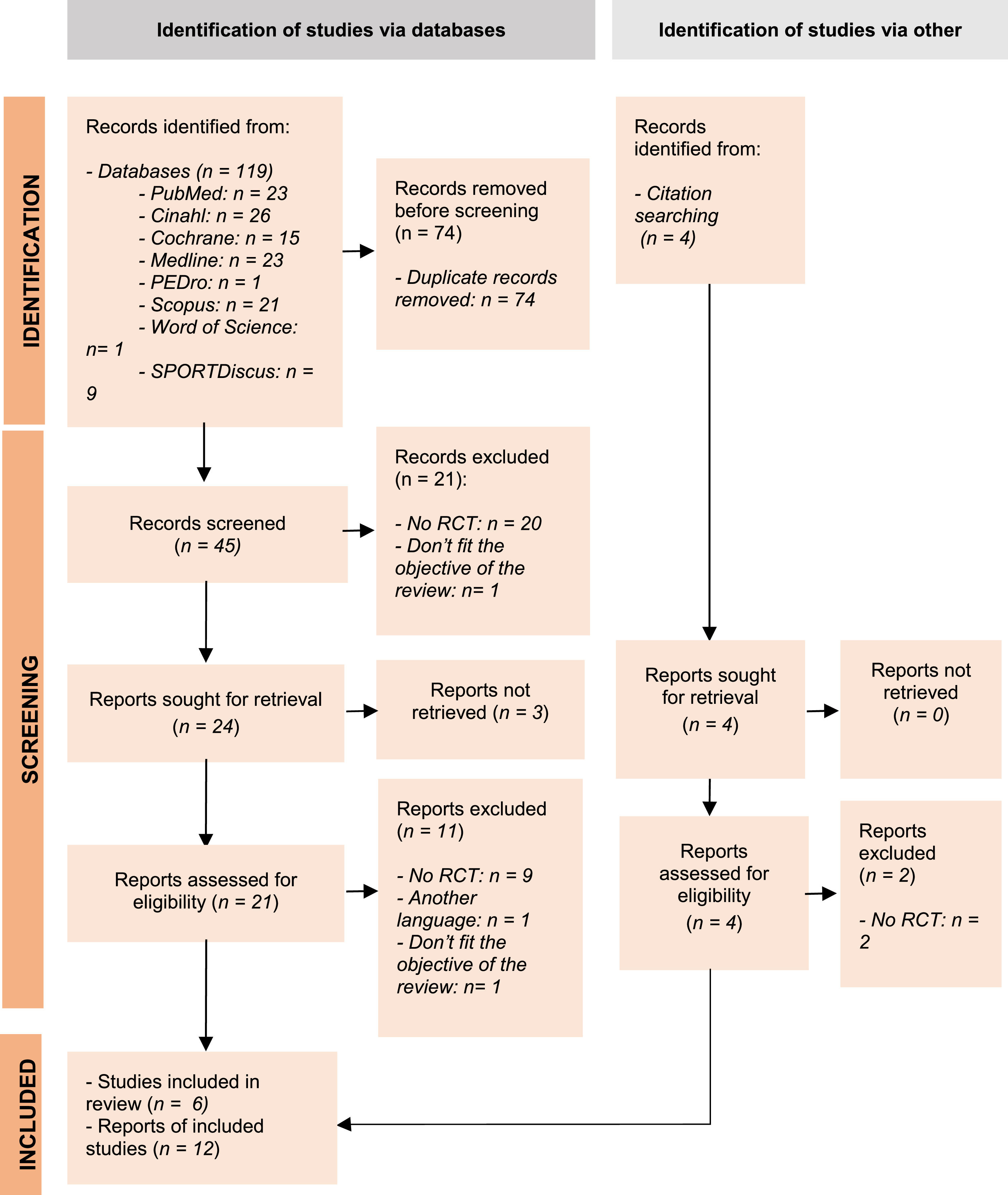
ResultsThe total number of records identified by the database search was 119. Of the 119, 74 were eliminated as duplicate records. After applying the inclusion and exclusion criteria, the number of studies selected for the systematic review was 10.
In addition, 4 records were identified through manual citation searching, of which only 2 met the selection criteria established for this review. Together with the former, the total number of articles included in the synthesis was 12 (see Fig. 1).
Several of the selected studies19–25 stemmed from a trial presented by White et al.26 in 2013 called the Anterior Cruciate Ligament - Specialized Post-Operative Return To Sports (ACL-SPORTS) trail. The aim of the study was to analyze the effects of the EPS in combination with specialized post-operative training on the return to sport. Different lines of research were derived from this project, which resulted in seven scientific publications. A total of 6 studies and 12 articles have been published.
All studies sought to determine the efficacy of perturbation training as a method of neuromuscular re-education in individuals with a complete ACL tear or ACL graft. This was the main criterion for inclusion in the samples. In all cases, except Beard et al.,27 83% of the studies, the participants were athletes or individuals engaged in level I (e.g., football, football, basketball) or level II (e.g., racquet sports, skiing, heavy physical work) physical activities according to the International Knee Documentation Committee (IKDC)28 for more than 50 h per year.19–25,29–32
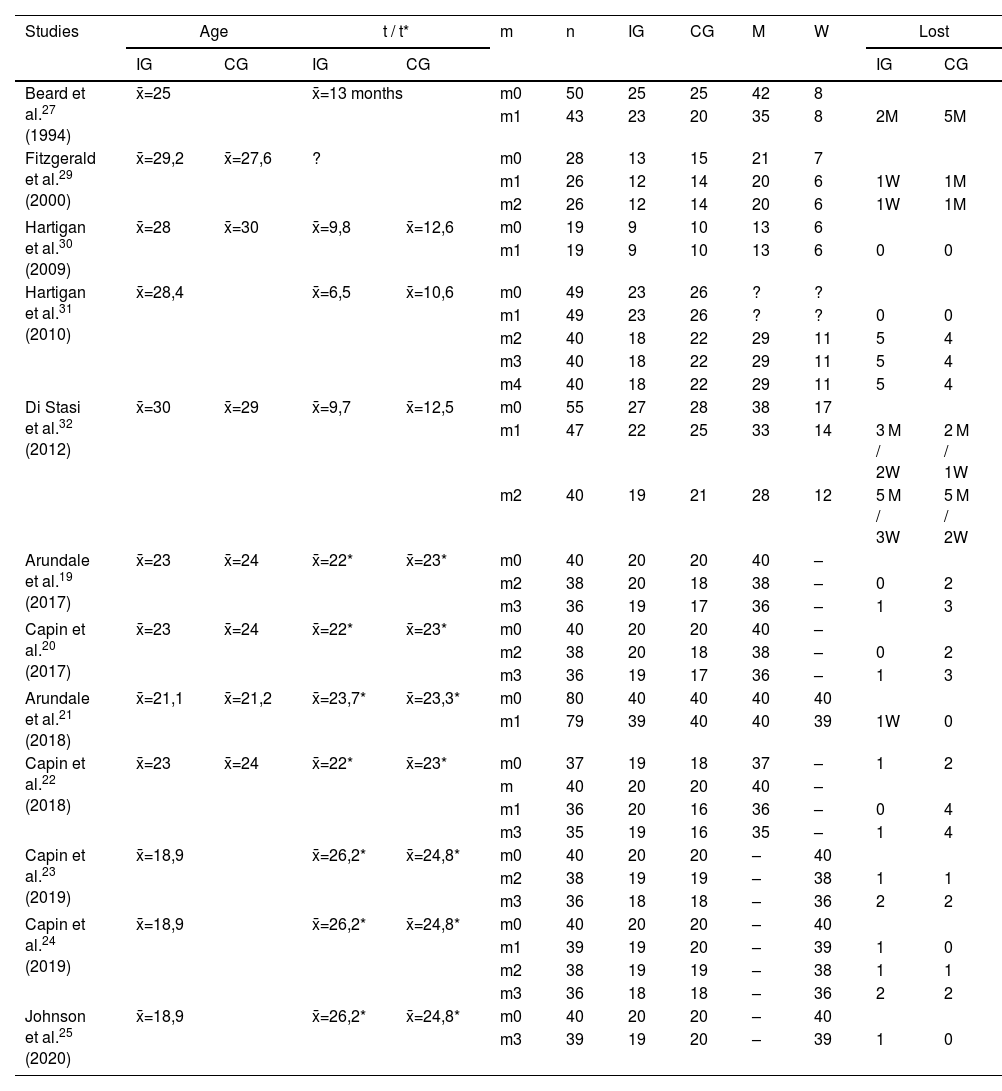
Table 3 summarizes the main characteristics of the samples.
Characteristics of the sample.
| Studies | Age | t / t* | m | n | IG | CG | M | W | Lost | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IG | CG | IG | CG | IG | CG | |||||||
| Beard et al.27 (1994) | x̄=25 | x̄=13 months | m0 | 50 | 25 | 25 | 42 | 8 | ||||
| m1 | 43 | 23 | 20 | 35 | 8 | 2M | 5M | |||||
| Fitzgerald et al.29 (2000) | x̄=29,2 | x̄=27,6 | ? | m0 | 28 | 13 | 15 | 21 | 7 | |||
| m1 | 26 | 12 | 14 | 20 | 6 | 1W | 1M | |||||
| m2 | 26 | 12 | 14 | 20 | 6 | 1W | 1M | |||||
| Hartigan et al.30 (2009) | x̄=28 | x̄=30 | x̄=9,8 | x̄=12,6 | m0 | 19 | 9 | 10 | 13 | 6 | ||
| m1 | 19 | 9 | 10 | 13 | 6 | 0 | 0 | |||||
| Hartigan et al.31 (2010) | x̄=28,4 | x̄=6,5 | x̄=10,6 | m0 | 49 | 23 | 26 | ? | ? | |||
| m1 | 49 | 23 | 26 | ? | ? | 0 | 0 | |||||
| m2 | 40 | 18 | 22 | 29 | 11 | 5 | 4 | |||||
| m3 | 40 | 18 | 22 | 29 | 11 | 5 | 4 | |||||
| m4 | 40 | 18 | 22 | 29 | 11 | 5 | 4 | |||||
| Di Stasi et al.32 (2012) | x̄=30 | x̄=29 | x̄=9,7 | x̄=12,5 | m0 | 55 | 27 | 28 | 38 | 17 | ||
| m1 | 47 | 22 | 25 | 33 | 14 | 3 M / 2W | 2 M / 1W | |||||
| m2 | 40 | 19 | 21 | 28 | 12 | 5 M / 3W | 5 M / 2W | |||||
| Arundale et al.19 (2017) | x̄=23 | x̄=24 | x̄=22* | x̄=23* | m0 | 40 | 20 | 20 | 40 | – | ||
| m2 | 38 | 20 | 18 | 38 | – | 0 | 2 | |||||
| m3 | 36 | 19 | 17 | 36 | – | 1 | 3 | |||||
| Capin et al.20 (2017) | x̄=23 | x̄=24 | x̄=22* | x̄=23* | m0 | 40 | 20 | 20 | 40 | – | ||
| m2 | 38 | 20 | 18 | 38 | – | 0 | 2 | |||||
| m3 | 36 | 19 | 17 | 36 | – | 1 | 3 | |||||
| Arundale et al.21 (2018) | x̄=21,1 | x̄=21,2 | x̄=23,7* | x̄=23,3* | m0 | 80 | 40 | 40 | 40 | 40 | ||
| m1 | 79 | 39 | 40 | 40 | 39 | 1W | 0 | |||||
| Capin et al.22 (2018) | x̄=23 | x̄=24 | x̄=22* | x̄=23* | m0 | 37 | 19 | 18 | 37 | – | 1 | 2 |
| m | 40 | 20 | 20 | 40 | – | |||||||
| m1 | 36 | 20 | 16 | 36 | – | 0 | 4 | |||||
| m3 | 35 | 19 | 16 | 35 | – | 1 | 4 | |||||
| Capin et al.23 (2019) | x̄=18,9 | x̄=26,2* | x̄=24,8* | m0 | 40 | 20 | 20 | – | 40 | |||
| m2 | 38 | 19 | 19 | – | 38 | 1 | 1 | |||||
| m3 | 36 | 18 | 18 | – | 36 | 2 | 2 | |||||
| Capin et al.24 (2019) | x̄=18,9 | x̄=26,2* | x̄=24,8* | m0 | 40 | 20 | 20 | – | 40 | |||
| m1 | 39 | 19 | 20 | – | 39 | 1 | 0 | |||||
| m2 | 38 | 19 | 19 | – | 38 | 1 | 1 | |||||
| m3 | 36 | 18 | 18 | – | 36 | 2 | 2 | |||||
| Johnson et al.25 (2020) | x̄=18,9 | x̄=26,2* | x̄=24,8* | m0 | 40 | 20 | 20 | – | 40 | |||
| m3 | 39 | 19 | 20 | – | 39 | 1 | 0 | |||||
CG: control group. GI: intervention group. M: men. m: moment. W: women. n: sample size. t: time between injury and intervention (weeks). t*: time between surgery and intervention (weeks). x̄: mean.
As for the age range of the subjects participating in the trials, it ranged from a minimum19,20–25,31,32 of 13 years to a maximum29 of 57 years.
Regarding exclusion criteria, 100% of the studies excluded cases with concomitant grade III injury of other knee ligaments, 83% of the studies (5 out of 6) excluded subjects with severe chondral injury19–25,27,30–32 (4 of them specify "full-thickness chondral injury greater than 1 cm), but only 50% of the studies excluded subjects with complex and/or repairable meniscal tear.27,29,30 The ACL-SPORTS trial, which represents 16% of the studies and 53% of the articles included in this synthesis, also excluded individuals with a previous history of RACL or severe injury in the same or contralateral lower limb.
Regarding treatment, in only 33% of the studies was the conservative approach the therapeutic option of choice and participants did not undergo ACL reconstruction surgery.27,29 In the other 66%, a surgical approach in combination with physiotherapeutic treatment was chosen.19–25,30–32 In the ACL-SPORTS trial19–25 the intervention under analysis took place after ligament reconstruction, while in the remaining studies30–32 the intervention was prior to surgery. In the latter case, Hartigan et al.30,31 analyzed in their trials the influence of PBBT on postoperative outcomes. However, Di Stasi et al.32 went further and analyzed the results both before surgery, i.e. at the end of surgery, and 6 months after reconstruction.
In most of the trials in this review, the participating subjects completed a basic training protocol, both in the intervention group (IG) and in the control group (CG), in which muscle strength work for the lower limb was the common denominator. Thus, Fitzgeral et al.29 included in their protocol resisted exercises for quadriceps and hamstrings, cardiovascular endurance training, and agility and sport-specific skills training. Hartigan et al.30,31 performed progressive training to increase quadriceps strength following the American College of Sports Medicine guidelines. Di Stasi et al.32 opted for a criteria-based strength protocol featuring closed kinetic chain, open kinetic chain, isokinetic and neuromuscular electrostimulation exercises. Finally, in the articles belonging to the ACL-SPORTS19–25 trial, the basic training consisted of strength, agility, plyometric and secondary prevention (SAPP) exercises.
To this baseline training, perturbation-based balance training was added for the IG, with minor variations between the trials analyzed. Fitzgerald et al.29 proposed a program based on 4 techniques: balance perturbations on a motorized force platform, perturbations on a rocking board, perturbations with one foot on a stable platform and the other on a board with wheels, and perturbations in monopodial support on a board with wheels. Based on this proposal, but without the force platform, the same authors published the guidelines for the University of Delaware Disturbance Training Programme (UDPT)9 that would serve as a guide for the remaining trials in this review.19–25,30–32 In the case of the ACL-SPORTS study19–25 the CG patients, unlike the GI patients, performed an additional single-leg balance exercise with additional resistance to the hip flexors of the sound limb.
Only Beard et al.27 performed a strict comparison between a traditional treatment regimen for CG and a proprioceptive training regimen exclusively for IG. In this study, although they did not use the term "perturbation training" as such, they did include for their CG exercises on moving or unstable surfaces inspired by the proposal made by Ihara and Nakayama33 in 1986.
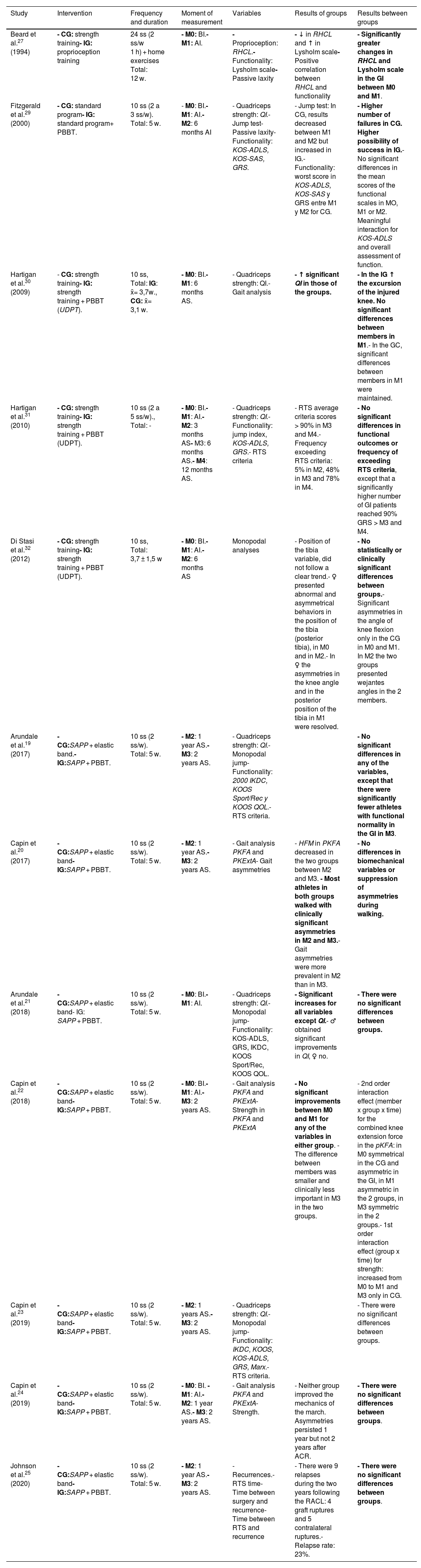
Table 4 summarizes the characteristics of the interventions carried out, the variables measured per study and the results obtained.
Characteristics of the interventions, moments of measurement, variables and results.
| Study | Intervention | Frequency and duration | Moment of measurement | Variables | Results of groups | Results between groups |
|---|---|---|---|---|---|---|
| Beard et al.27 (1994) | - CG: strength training- IG: proprioception training | 24 ss (2 ss/w 1 h) + home exercises Total: 12 w. | - M0: BI.- M1: AI. | - Proprioception: RHCL.- Functionality: Lysholm scale- Passive laxity | - ↓ in RHCL and ↑ in Lysholm scale- Positive correlation between RHCL and functionality | - Significantly greater changes in RHCL and Lysholm scale in the GI between M0 and M1. |
| Fitzgerald et al.29 (2000) | - CG: standard program- IG: standard program+ PBBT. | 10 ss (2 a 3 ss/w). Total: 5 w. | - M0: BI.- M1: AI.- M2: 6 months AI | - Quadriceps strength: QI.- Jump test- Passive laxity- Functionality: KOS-ADLS, KOS-SAS, GRS. | - Jump test: In CG, results decreased between M1 and M2 but increased in IG.- Functionality: worst score in KOS-ADLS, KOS-SAS y GRS entre M1 y M2 for CG. | - Higher number of failures in CG. Higher possibility of success in IG.- No significant differences in the mean scores of the functional scales in MO, M1 or M2. Meaningful interaction for KOS-ADLS and overall assessment of function. |
| Hartigan et al.30 (2009) | - CG: strength training- IG: strength training + PBBT (UDPT). | 10 ss, Total: IG: x̄= 3,7 w., CG: x̄= 3,1 w. | - M0: BI.- M1: 6 months AS. | - Quadriceps strength: QI.- Gait analysis | - ↑ significant QI in those of the groups. | - In the IG ↑ the excursion of the injured knee. No significant differences between members in M1.- In the GC, significant differences between members in M1 were maintained. |
| Hartigan et al.31 (2010) | - CG: strength training- IG: strength training + PBBT (UDPT). | 10 ss (2 a 5 ss/w)., Total: - | - M0: BI.- M1: AI.- M2: 3 months AS- M3: 6 months AS.- M4: 12 months AS. | - Quadriceps strength: QI.- Functionality: jump index, KOS-ADLS, GRS.- RTS criteria | - RTS average criteria scores > 90% in M3 and M4.- Frequency exceeding RTS criteria: 5% in M2, 48% in M3 and 78% in M4. | - No significant differences in functional outcomes or frequency of exceeding RTS criteria, except that a significantly higher number of GI patients reached 90% GRS > M3 and M4. |
| Di Stasi et al.32 (2012) | - CG: strength training- IG: strength training + PBBT (UDPT). | 10 ss, Total: 3,7 ± 1,5 w | - M0: BI.- M1: AI.- M2: 6 months AS | Monopodal analyses | - Position of the tibia variable, did not follow a clear trend.- ♀ presented abnormal and asymmetrical behaviors in the position of the tibia (posterior tibia), in M0 and in M2.- In ♀ the asymmetries in the knee angle and in the posterior position of the tibia in M1 were resolved. | - No statistically or clinically significant differences between groups.- Significant asymmetries in the angle of knee flexion only in the CG in M0 and M1. In M2 the two groups presented wejantes angles in the 2 members. |
| Arundale et al.19 (2017) | - CG:SAPP + elastic band.- IG:SAPP + PBBT. | 10 ss (2 ss/w). Total: 5 w. | - M2: 1 year AS.- M3: 2 years AS. | - Quadriceps strength: QI.- Monopodal jump- Functionality: 2000 IKDC, KOOS Sport/Rec y KOOS QOL.- RTS criteria. | - No significant differences in any of the variables, except that there were significantly fewer athletes with functional normality in the GI in M3. | |
| Capin et al.20 (2017) | - CG:SAPP + elastic band- IG:SAPP + PBBT. | 10 ss (2 ss/w). Total: 5 w. | - M2: 1 year AS.- M3: 2 years AS. | - Gait analysis PKFA and PKExtA- Gait asymmetries | - HFM in PKFA decreased in the two groups between M2 and M3. - Most athletes in both groups walked with clinically significant asymmetries in M2 and M3.- Gait asymmetries were more prevalent in M2 than in M3. | - No differences in biomechanical variables or suppression of asymmetries during walking. |
| Arundale et al.21 (2018) | - CG:SAPP + elastic band- IG: SAPP + PBBT. | 10 ss (2 ss/w). Total: 5 w. | - M0: BI.- M1: AI. | - Quadriceps strength: QI.- Monopodal jump- Functionality: KOS-ADLS, GRS, IKDC, KOOS Sport/Rec, KOOS QOL. | - Significant increases for all variables except QI.- ♂ obtained significant improvements in QI, ♀ no. | - There were no significant differences between groups. |
| Capin et al.22 (2018) | - CG:SAPP + elastic band- IG:SAPP + PBBT. | 10 ss (2 ss/w). Total: 5 w. | - M0: BI.- M1: AI.- M3: 2 years AS. | - Gait analysis PKFA and PKExtA- Strength in PKFA and PKExtA | - No significant improvements between M0 and M1 for any of the variables in either group. - The difference between members was smaller and clinically less important in M3 in the two groups. | - 2nd order interaction effect (member x group x time) for the combined knee extension force in the pKFA: in M0 symmetrical in the CG and asymmetric in the GI, in M1 asymmetric in the 2 groups, in M3 symmetric in the 2 groups.- 1st order interaction effect (group x time) for strength: increased from M0 to M1 and M3 only in CG. |
| Capin et al.23 (2019) | - CG:SAPP + elastic band- IG:SAPP + PBBT. | 10 ss (2 ss/w). Total: 5 w. | - M2: 1 years AS.- M3: 2 years AS. | - Quadriceps strength: QI.- Monopodal jump- Functionality: IKDC, KOOS, KOS-ADLS, GRS, Marx.- RTS criteria. | - There were no significant differences between groups. | |
| Capin et al.24 (2019) | - CG:SAPP + elastic band- IG:SAPP + PBBT. | 10 ss (2 ss/w). Total: 5 w. | - M0: BI. - M1: AI.- M2: 1 year AS.- M3: 2 years AS. | - Gait analysis PKFA and PKExtA- Strength. | - Neither group improved the mechanics of the march. Asymmetries persisted 1 year but not 2 years after ACR. | - There were no significant differences between groups. |
| Johnson et al.25 (2020) | - CG:SAPP + elastic band- IG:SAPP + PBBT. | 10 ss (2 ss/w). Total: 5 w. | - M2: 1 year AS.- M3: 2 years AS. | - Recurrences.- RTS time- Time between surgery and recurrence- Time between RTS and recurrence | - There were 9 relapses during the two years following the RACL: 4 graft ruptures and 5 contralateral ruptures.- Relapse rate: 23%. | - There were no significant differences between groups. |
PBBT: Perturbation-based balance training. BI: Before intervention. AS: After surgery. AI: after intervention. CG: Control group. IG: Intervention group. GRS: global rated scale. HFM: hip flexion movement. IKDC 2000: International knee documentation. KOOS Sport: The Knee injury and Osteoarthritis Outcome Score-sports. KOOS QOL: The Knee injury and Osteoarthritis Outcome Score-quality of life. KOS-ADLS: knee outcome survey-daily life. KOS-SAS: knee outcome survey. ACL: Anterior cruciate ligament. PKFA: peak of knee flexion angle. PKExtA: peak of knee extension angle. QI: quadriceps index. RTS: Return to sport. RHCL: Reflect hamstring contraction latency. RACL: Reconstruction of anterior cruciate ligament. SAPP: Strength, agility, prevention and plyometrics. W: weeks. Ss: Sessions. UDPT: University of Delaware for PBBT.
Depending on the variables measured in each article, they can be grouped into three different typologies. Firstly, articles that assess the functional level of the patient19,21,23,27,29,31 by measuring parameters such as isometric quadriceps strength19,21,23,29,31 (quadriceps index, QI), the ability to jump with one foot19,21,23,29,31 (single jump, cross jump, triple jump and 6 m) or the functionality perceived by the patient19,21,23,27,29,31 (self-administered questionnaires: Lysholm, 2000 IKDC, KOOS Sport/Rec and KOOS QOL, GRS, KOS-ADLS, Marx). Some of these publications also measure the ability of subjects to recover their pre-injury level of activity using variables such as the proportion of individuals passing the criteria for RTS19 or the time taken to pass the criteria.23 They account for 50% of the articles in this review. Secondly, articles assessing the kinetics and kinematics of the knee and/or hip,20,22,24,30,32 in which parameters such as joint angles,20,22,24 tibial position,32 joint excursions during gait,20,24,30,32 force moments20,22 and joint contact forces22,24 are measured. In most cases, they are intended to show the presence, or not, of asymmetries between the injured limb and the sound limb. They account for 41.6% of the publications in this review. Finally, articles that evaluate the recurrence of the injury, for which they use variables such as the number of relapses and their characteristics (laterality, surgical technique), the recurrence rate, the time from surgery to relapse and the time from the RTS to the new rupture. We have only one example among the selected publications, Johnson et al.,25 8.3% of the total.
Beard et al.27 observed a reduction in mean hamstring reflex contraction latency (RHCL) and an increase in mean Lysholm scale score in both groups, although the changes were significantly greater in the GI (p < 0.05 for RHCL and p < 0.005 for Lysholm). In both groups, there was a positive correlation between improvement in RHCL and functional improvement (p < 0.05).
Fitzgerald et al.29 found that the number of individuals who failed to recover was significantly higher in the CG (p < 0.05), with a 4.88 times higher probability of success in the IG. Scores for the long jump and triple jump were significantly higher in the IG 6 months after the intervention (p < 0.05) and a positive interaction was observed in scores on the cross-jump test (p < 0.05), in favor of the IG. In addition, while there were no significant between-group differences in mean scores on the functional scales, there was a significant interaction over time between the end of training and 6 months later for the KOS-ADLS scale (p < 0.03) and global knee function assessment (p < 0.03), in favor of the IG.
In their 2009 study, Hartigan et al.30 observed that quadriceps strength ratings increased significantly for both groups 6 months after RACL (p = 0.002). In terms of knee excursion during the mid-stance phase of gait, subjects who received PBBT prior to surgery (GI) had no significant differences 6 months after surgery (p = 0.14), whereas subjects who received strength training only (SC) did maintain significant differences between the two limbs (p = 0.007), with knee excursion being lower in the injured limb.
One year later, Hartigan et al.31 found that there was no difference in functional outcomes between the two groups or in the number of patients who passed all RTS criteria. The only exception was that a significantly higher percentage of IG subjects achieved the necessary score on the GRS to pass the criteria for return to sport, 6 and 12 months after surgery (p = 0.025 and p = 0.04, respectively). Mean scores for each functional outcome met RTS criteria 6 and 12 months after surgery. However, based on individual data counts, the frequency of success was 5% at 3 months, 48% at 6 months and 78% at 12 months.
In the analysis of the single-foot stance task by Di Stasi et al.,32 neither group demonstrated a clear pattern of adaptation to preoperative treatment. There were no statistically or clinically significant differences between groups in mid tibial position or knee flexion angle in any of the measurements. Only in the CG were there significant asymmetries (p = 0.004) in knee flexion angle preoperatively that persisted postoperatively (p = 0.001). These inter-limb differences appeared resolved 6 months after surgery. In the analysis by sex, men and women seem to respond differently to surgical and physiotherapeutic treatment. Thus, women may have a better response to preoperative therapy as the initial asymmetries in knee angle and posterior tibial position resolved after surgery.
Arundale et al.,19 in their report on functional outcomes in men in the ACL-SPORTS trial, observed no significant differences between groups in any of the variables analysed, with the exception of the number of athletes with functional normality 2 years after surgery, which was lower in the IG (p = 0.03).
Capin et al.20 found no significant differences between treatment groups for any of the biomechanical gait variables. There was also no difference in the proportion of athletes in whom limb-to-limb asymmetries disappeared; most athletes in both groups walked with clinically significant asymmetries between the two limbs, both 1 and 2 years after RACL. Even so, when comparing the mean differences between limbs for each group, gait asymmetries were more prevalent 1 year later.
In 2018 Arundale et al.21 observed significant (p < 0.01) pre- and post-intervention increases in mean values for all variables except QI, although with no differences between treatment groups. In analysis by sex, both men and women had significant improvements in all measures of knee function (p < 0.01) and patient-reported measures (p < 0.01 for all except KOS-ADL in women, p = 0.02) except QI, which increased significantly in men (p = 0.02) but not in women (p = 0.086).
The results of the study by Capin et al.22 showed no significant improvements in the short term (between pre-training and post-training) in either treatment group. Overall, maximal knee flexion angle, maximal extension moment, combined extensor muscle strength, medial compartment contact force and tibiofemoral contact force were lower in the injured limb in each group over time. However, the magnitude of the differences between limbs was minor and probably of no clinical significance 2 years after surgery.
In another study, Capin et al.23 found not statistically or clinically significant differences between the two groups for any of the functional variables measured in the sample of female athletes in the ACL-SPORTS trial.
In the analysis of gait mechanics that Capin et al.24 performed on the same sample of female athletes, there were also no clinically significant interactions by group. Neither IG nor CG improved gait mechanics immediately after the intervention. Asymmetrical movement patterns persisted 1 year after RACL but appeared to resolve 2 years later, particularly regarding sagittal plane knee kinetics and kinematics.
Johnson et al.25 reported 9 relapses during the 2 years after ACLR among the cohort of women in the ACL-SPORTS trial: 4 graft ruptures (all hamstring autografts) and 5 contralateral ACL ruptures. The overall relapse rate was 23%. However, there were no significant differences between groups in either the relapse rate or the side of the second injury.
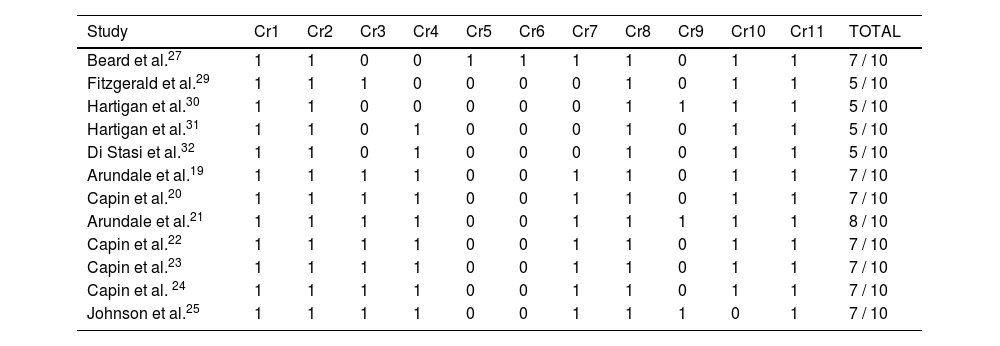
Regarding the methodological quality of the review articles, the lowest score was 5 points in 33.3% of the cases29–32 (4 out of 12). The most repeated score was 7 points in 58.3% of the articles19,20,22–25,27 and in only one article21, 8.3%, the total was 8 points. Table 5 in the appendix shows the score per criterion analyzed and the total score achieved on the PEDro scale.
Methodological quality according to PEDro scale.
| Study | Cr1 | Cr2 | Cr3 | Cr4 | Cr5 | Cr6 | Cr7 | Cr8 | Cr9 | Cr10 | Cr11 | TOTAL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beard et al.27 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 7 / 10 |
| Fitzgerald et al.29 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 / 10 |
| Hartigan et al.30 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 / 10 |
| Hartigan et al.31 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 / 10 |
| Di Stasi et al.32 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 / 10 |
| Arundale et al.19 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 / 10 |
| Capin et al.20 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 / 10 |
| Arundale et al.21 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 / 10 |
| Capin et al.22 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 / 10 |
| Capin et al.23 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 / 10 |
| Capin et al. 24 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 / 10 |
| Johnson et al.25 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 7 / 10 |
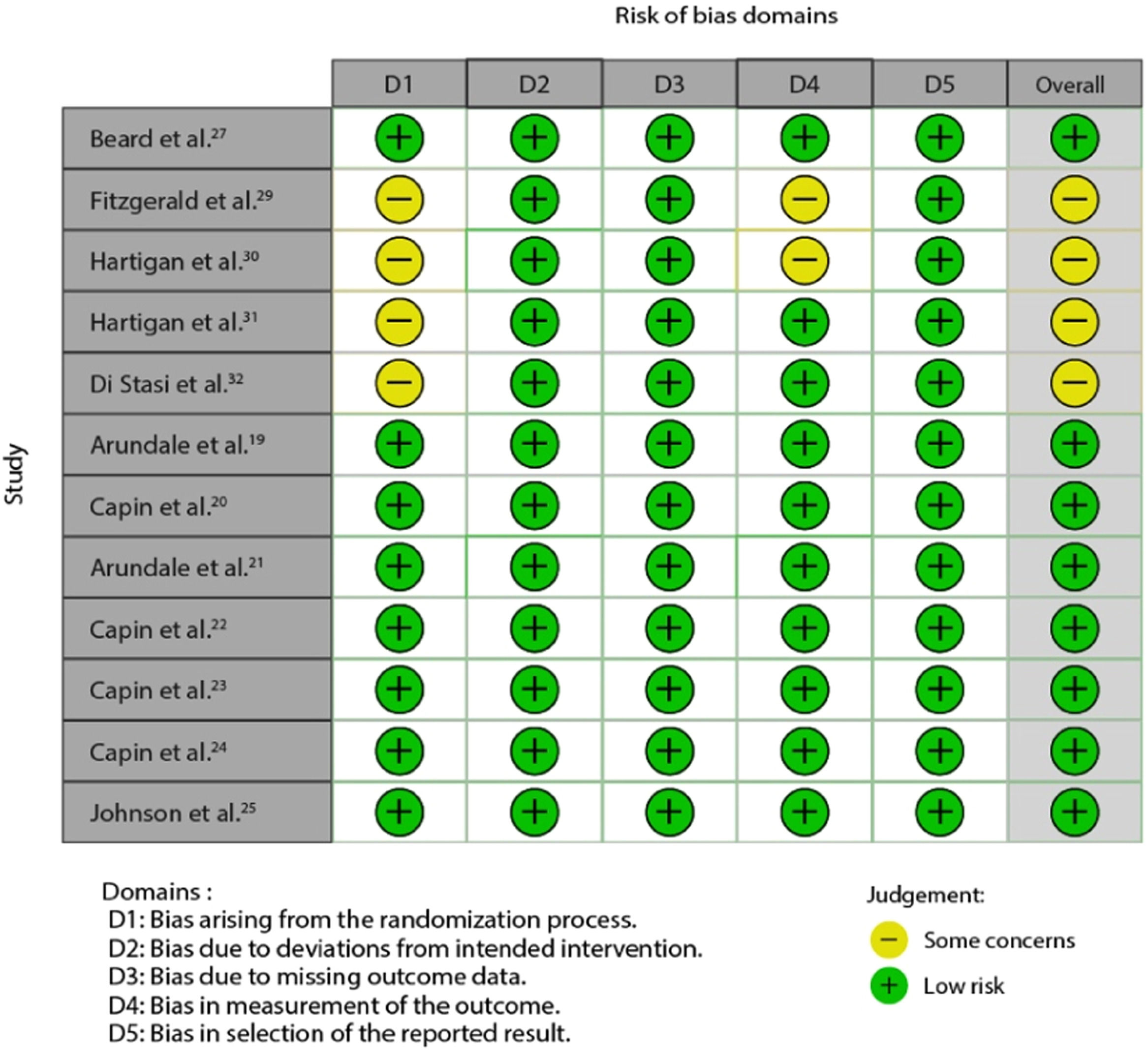
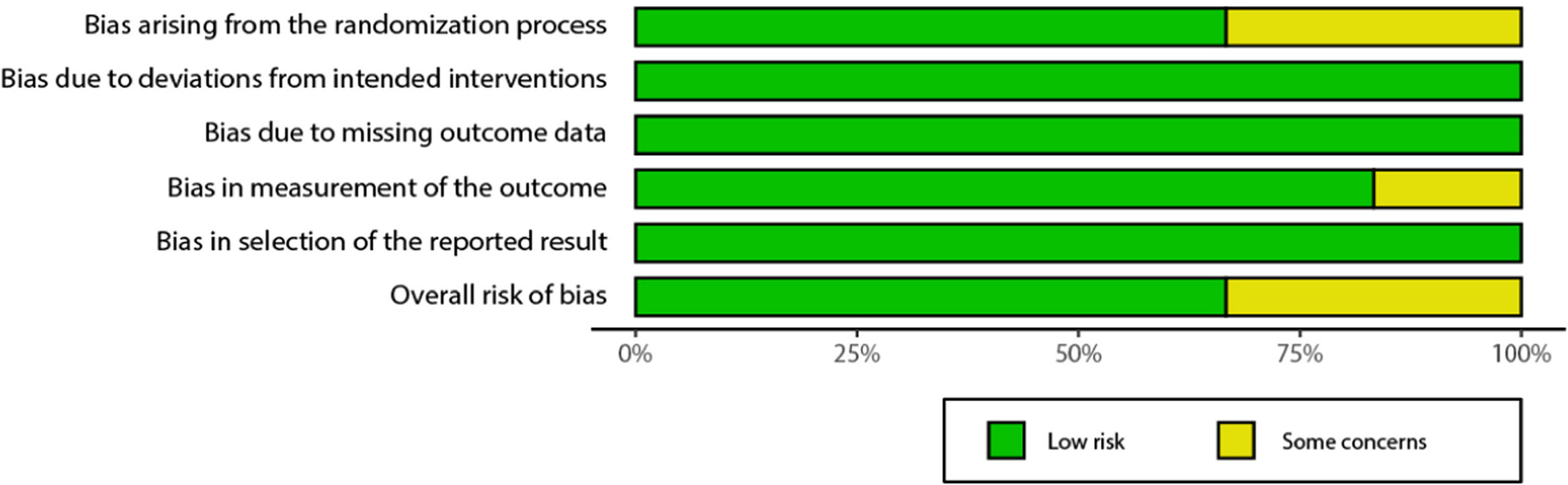
In the risk of bias analysis according to the RoB 2 tool, 8 of the 12 articles, or 66.6%, achieve an overall rating of "Low risk "18–24.26. The remaining 33% have "some concerns"28–31 mainly due to the randomization process followed during the sample selection phase. Figs. 2 and 3 in the annex show the results obtained using a traffic light graph and a bar chart, respectively.
DiscussionWhen commenting on the findings of this review, it is necessary to divide the selected studies into two groups: those in which the participating subjects underwent conservative treatment and those in which they underwent RACL surgery.
Among those who followed the conservative therapeutic option,27,29 the results obtained were positive for the experimental group, in both cases. Thus, Fitzgerald et al.29 found that including the PBBT in non-surgical ACL rehabilitation programs increased the probability of success in returning to high-level physical activity in patients classified as copers, or potentially tolerant. According to the authors themselves, although the mechanism of action cannot be derived from the study results, additional exposure to destabilizing forces in a controlled and progressive manner could result in the development of compensatory patterns of muscle activity. This point seems to be confirmed by subsequent studies34,35 showing that perturbation training increases movement and decreases muscle co-contractions in the involved limb during the weight-acceptance phase of gait. The result is improved coordination between quadriceps activity and hamstring and soleus activity that contributes to improved dynamic knee stability in a select population of individuals with ACL rupture, the so-called copers. Previously, Beard et al.27 already established that proprioceptive enhancement techniques, including base-of-support destabilizing exercises, were more effective in improving hamstring reflex contraction function and latency than traditional strengthening exercises. Along the same lines, Ihara and Nakayama33, pioneers in the use of unstable bearing surfaces to exercise dynamic knee control, observed a significant improvement in hamstring reaction time in the experimental group compared to the control group, supporting the theory that it is not only strength, but the ability of muscles to function quickly and adequately, that is related to joint stability and its improvement requires training.36
Among the trials in which the study subjects underwent RACL surgery, we found a subgroup30–32 of three in which intervention using perturbation techniques takes place prior to surgery. All three have in common that the target population are subjects classified as non-copers according to the criteria established by Fitzgerald et al.37 That is, subjects who, due to the characteristics of their lesion, are not candidates for conservative management. On the one hand, Hartigan et al.30 confirmed their initial hypothesis that non-copers who received PBBT would show greater symmetry in knee excursion during the mid-stance phase of gait 6 months after surgery. However, the strength training-only group continued to show less knee excursion in the injured limb. These between-group differences are consistent with those observed by Chmielewski35 in copers. In contrast, in the study published in 2010, Hartigan et al.31 found no significant differences between groups in postoperative functional outcomes, with the only exceptions being that patients in the control group jumped faster at 12 months and those in the intervention group rated knee function (by GRS scale) more favorably 6 and 12 months after RACL. The high mean scores achieved by the two groups at 6 months after surgery (the means for all functional outcomes exceeded the 90% cutoff) contrast with the 52% of subjects who did not pass the 7 criteria established by the same authors for RTS. One of the reasons, according to Hartigan et al.31 could be the high demands of these criteria. Nevertheless, the trial results point to the importance of assessing each athlete on an individual basis rather than basing RTS on temporal criteria, as non-copers may require a longer period of supervised physical therapy before returning to pre-injury function.
Di Stasi et al.32 agree that non-copers constitute a very diverse group, with different adaptive capacity among individuals, which is reflected in the diversity of results achieved after the intervention. In their trial, none of the study groups demonstrated a clear pattern of adaptation to preoperative treatment. Beyond the between-group results, the authors suggest sex-specific kinematic responses within the non-coper cohort. Women seem to be more sensitive to preoperative neuromuscular training programs, such as PBBT, and adopt more symmetrical patterns between limbs in static tasks such as single-foot stance32 but also in dynamic tasks such as gait38.
In view of the results obtained in non-copers, it appears that preoperative perturbation training combined with progressive quadriceps strengthening did not improve their ability to return to sport compared to strength training alone but was effective in normalizing postoperative knee excursion.13 As interpreted by Hartigan et al.30 PBBT may improve gamma loop feedback and decrease antagonistic muscle activity, thereby improving the ability of the quadriceps to dynamically stabilize the knee during gait.
The ACL-Specialized Post-Operative Return To Sports (ACL-SPORTS) trial26 set out to investigate whether applying PBBT after ACLR surgery could be successful in resolving postoperative deficits that contribute to poor functional outcomes and increased risk of secondary ACL injuries.
Attending to clinical and functional outcomes, Arundale et al.19,21 and Capin et al.23 concur that the postoperative SAPP-type training program improved functional outcomes and activity levels among athletes after RACL, and this was true regardless of whether specific perturbation training was added. The scores obtained on subjective rating scales were higher than those published in previous literature such as or Scandinavian ACL registry38 one year after surgery, indicating that the program may be a valuable intervention in the return-to-sport phase.21
In the gender comparison, men and women obtained significant improvements in all subjective rating scales and jumping tests. However, in the quadriceps symmetry index (QI), only men experienced significant increases even though both sexes had similar values before the intervention. During the RTS phase, it is common for clinical physiotherapists to shift their focus to the training of specific movements and sports skills, neglecting previous aspects such as quadriceps strength.21 On the contrary, the results of the study by Arundale et al.21 suggest that women need to prolong a specific part of their rehabilitation focused on quadriceps strengthening. This is a factor to be considered given the relationship between QI and the risk of relapse since, as noted by Grindem et al.39, a 1% increase in quadriceps strength symmetry leads to a 3% reduction in the risk of relapse.
Regarding the analysis of gait kinetics and kinematics and joint contact forces, none of the training typologies, with or without PBBT, seems to be effective in improving gait mechanics in the short and medium term, regardless of gender. The 3 studies conducted by Capin et al.20,22,24 concur that most of the observed asymmetries in gait pattern largely persist up to 2 years after ligament reconstruction, long after patients achieve symmetry in quadriceps strength and knee functionality and have even regained sporting activity. These findings help to reinforce a growing body of evidence suggesting that full recovery after RACL may take longer than previously thought. Along these lines Roewer et al.40 report improvement in quadriceps strength and asymmetric movement patterns 2 years after surgery among the non-coper cohort. Kauer et al.41 go even further and conclude, after a systematic review of 40 studies and meta-analysis of 27, that complete restoration of knee kinematics during gait takes an average of almost 6 years.
Regarding the rate of ACL injury recurrence, Johnson et al.25 state that although the addition of the PBBT to a secondary prevention program does not appear to be of major benefit to female athletes, the rate of contralateral ACL injury (14.3% under 25 years of age) was lower42,43 or comparable to that reported by previous research.44 However, the overall recurrence rate, 23.1%, was much higher than that reported among men. According to Arundale et al.,45 the relapse rate for men in the ACL-SPORTS trial was only 2.5% within 2 years after RACL, with only one case of secondary injury due to allograft rupture. The reduction in cases of recurrence among women compared to other publications reaffirms the importance of instituting a secondary prevention program in the RTS phase. Similarly, Wiggins et al.46 argue that activity modification, improved rehabilitation and return-to-sport patterns coupled with the use of integrative neuromuscular training may help athletes reintegrate into sport more safely and reduce secondary injuries among the at-risk population. Even so, the ACL-SPORTS trial training program does not appear sufficient to address the needs of female athletes, who continue to have high relapse rates, making further research in this area necessary.
In general, it is noted that none of the studies derived from the ACL-SPORTS trial26 found significant differences between IG and CG, so it can be concluded that the PBBT does not provide an additional benefit to the SAPP program in rehabilitation after RACL surgery. The causes for the lack of results may be several. First, the trial includes a diversity of surgical techniques with different types of grafts and practiced by different surgeons, which makes the sample more heterogeneous and representative of a real clinical population, but also introduces variability factors.24 Second, there was no control for pre- or postoperative rehabilitation prior to the start of the study; the factor for homogenization of the sample was the inclusion criteria.21 Third, the high stringency of these same selection criteria, which leaves little room for improvement. And fourth, both study groups followed a specialized RTS training program, but in the case of the IG, perturbation training was added. If, as demonstrated, SAPP-type training alone is capable of positively modifying any of the variables measured, we would be faced with a possible "ceiling effect" that masks the real contribution of the PBBT.19 Such an effect would be avoided by exclusively comparing the PBBT with another type of treatment/training or placebo.20
Half of the studies included in the review21,27,29–32 chose mixed samples of men and women, although there was a marked preponderance of the male sex. Although the authors of the studies do not provide an explanation for this imbalance, it can be assumed to be due to a lower presence of female athletes in the target population. To avoid this, Arundale et al.21 carried out a stratified randomization by sex and, in this way, ensured an equal number of men and women in their sample. Of the remaining studies, all belonging to the ACL-SPORTS trial, 3 focused only on men19,20,22 and another 3 on women,23–25 observing a parallelism in the variables analyzed to ensure comparison between sexes.
The age of the subjects was homogeneous. The mean of almost all the studies19–22,29–32 was between 20 and 30 years of age. It should be considered that one of the common inclusion criteria was the habitual practice of physically demanding activities (IKDC level 1 or 2). Only the studies on the female population had a mean age below 20 years, specifically 18.9 years. This could have influenced the relapse figures if we consider that the rate is higher among younger athletes.46
The interventions in all the studies reviewed,19–25,29–32 with the sole exception of the trial by Beard et al.,27 were limited to 10 sessions in total, with a frequency of between 2 and 5 sessions per week. Sugimoto et al.47 suggest that the greater the volume, frequency, and duration of neuromuscular training sessions, the greater the efficacy in the primary prevention of knee injuries in female athletes. On this basis, it is conceivable that 10 sessions over 5 weeks may not maximize the benefits of PBBT. Further research is therefore needed on longer, higher intensity and more frequent secondary prevention programs, especially in women.25
Apart from Beard et al.,27 when applying the PBBT we followed the guidelines of the University of Delaware program9 which uses only three types of support surface: a plank with wheels, a static platform and an oscillating plank. In addition to these, other types of unstable surfaces are now available, such as a wobble board or a bosu-type device with a flat surface facing upwards.12,48,49 In the latter case, the PBBT is notably more challenging since it allows greater freedom of movement in all planes, so it could be thought that the results obtained would also be greater.12 Another option is the Balance Master motorized force platform, already used by Fitzgerald et al.29 or the Reactive Agility System, a mechanical device with a moving surface capable of providing standardized perturbations in the 3 planes of movement, which was used by Nawaresh et al.50–52 in their studies.
On the other hand, according to the UDPT protocol, the PBBT is performed in static positions, in monopodal or bipodal support, but not during gait or other types of dynamic situations common in sports practice. Apart from this, for athletes who practice contact sports such as soccer or basketball, the perturbations could be directed not only at the support surface but also at the body to simulate real game situations.12,53
The main limitation of this review lies in the fact that seven of the publications analyzed19–25 are based on the same experimental design.26 In addition, another four trials apply the same intervention protocol29–32 and share several authors. This gives homogeneity to the samples and intervention protocols, but, at the same time, detracts from the diversity of approach and external validity of the findings. Another limitation is the date on which the trials were conducted because, although the latest publications included date from 2019 to 2020, it should be considered that the ACL-SPORTS trial was approved in 2011, which could reduce the validity of the results obtained.
Thus, there is room for experimentation with new PBBT application protocols, with different dosages and updated perturbation and measurement devices, as well as efficacy comparisons with other neuromuscular re-education methods. Likewise, new avenues of research into strategies that help to shorten the time to full restoration of symmetry during gait, through direct and individualized treatment proposals that extend over months or even years, are assured.54,55 These proposals could be based on continuous monitoring and/or real-time feedback using wearable sensors and other technologies.22,56,57 In addition, the aforementioned gender differences in response to neuromuscular treatment open up a specific field of work among female athletes.
ConclusionsThe PBBT proved to be effective in the non-surgical recovery of potential tolerant patients or copers, improving joint stability and neuromuscular control. It was also effective as a preoperative treatment in non-copers in normalizing knee excursion after ACL reconstruction surgery. In contrast, the evidence reviewed does not support its efficacy as the neuromuscular re-education method of choice in the return to sport phase in previously operated athletes.