Bone-patellar tendon-bone (BPTB) autograft is the main treatment choice on complete anterior cruciate ligament (ACL) ruptures. However, high donor-site morbidity has been related to this procedure. A better understanding of the donor-site healing process could help us to decrease donor-site problems. The aim of this study is to describe the evolution of the patellar tendon size during the first year after BPTB procedure.
Materials and methods42 consecutive patients underwent ACL reconstruction using BPTB technique in our facilities. We measured the tendon length, width and thickness through musculoskeletal ultrasound before and at 1, 2, 4, 6, 9 and 12 months after the operation. Tendon measurements from the contralateral unaffected tendon were used as a control group. We compared the values between injured and uninjured legs and between pre-op and post-op values.
ResultsTendon length decreased significantly in both legs, without any difference between legs at 12 months post-op. Tendon width and thickness of the unaffected limbs showed a tendency to stabilization, while the injured limb showed a significant increase in both values during the first 1-2 months. At 12-months post-op, patellar tendon of the injured limb was significantly wider and thicker than the unaffected contralateral limb.
ConclusionHarvesting the central third of the patellar tendon during the BPTB procedure after an ACL injury leads to significant changes in the patellar tendon that can last for up to 12 months after the surgery. Further research must focus on the translation of these findings into clinical signs with longest follow-up periods.
Anterior cruciate ligament (ACL) injuries are one of the most important and severe lesions upon sport population, with 120,000 episodes annually registered in the United States1 and the longest time lost upon major soccer injuries.2 In cases of complete ACL tears, surgical reconstruction (ACLR) is the main choice of treatment, using several grafts to restore knee function and stability. From those, autograft bone-patellar tendon-bone (BPTB) is one of the most used, consisting on harvesting the central third of the patellar tendon to use it as ACL substitute.3 This procedure is highly popular due to its low rate of reinjury.4,5 However, BPTB technique has also been related to higher donor-site morbidity, involving anterior knee pain, loss of sensitivity or inability to kneeling.6–9
Defining the healing process at the patellar tendon is the first step to understand the causes of donor-site morbidity.10 As a part of that procedure, several authors have described the evolution of tendon size after harvesting its central third.11–13 Most of them have used radiographic or magnetic resonance imaging (MRI) due to its high sensitivity,6,14 but both are expensive methods that do not allow for continuous measurement. Musculoskeletal ultrasound (US) has been proposed as a simple, low-cost and valid method for patellar tendon evaluation, which allows continuous measurement.15,16
Prior researches have described the evolution of the patellar tendon size after ACLR.12,16 However, none of those have evaluated the differences on the patellar tendon size between injured and uninjured limbs during the first stages after ACLR. Thus, the aim of this study is to describe the evolution of the patellar tendon size obtained by US during the first year after ACLR and compare it with the contralateral unaffected patellar tendon.
MethodsDesignA prospective, single-centre, case series study was performed to compare the sonographic measurements of the patellar tendon between the injured and uninjured limbs during the first year after ACLR.
ParticipantsBetween January and December of 2009, 43 consecutive patients undergoing ACLR using BPTB technique were included in the study and followed-up for a year. All patients suffered an acute ACL injury diagnosed with both physical examination and MRI. The proposed treatment was reconstructive surgery at 6 weeks post-injury. Patients were aged between 19 and 49 years and had no history of previous surgery in either of both knees. They were excluded if presented a partial ACL rupture, had history of previous knee surgeries or showed any condition that made it impossible to perform US measurements. Patients were also excluded if they suffered any additional knee injury during the course of the study or had a history of contralateral knee surgery.
Surgical techniqueAll patients included in the study underwent ACLR with autologous BPTB graft performed by the same surgical team. The central third of the patellar tendon was taken from the injured knee together with bone plugs. After graft resection, the paratendon was sutured without closing the patellar tendon itself.
Sonographic measurementsBilateral sonographic measurements were taken before the surgery and at 1, 2, 4, 6, 8 and 12 months after the surgery by an expert physician (MR) on musculoskeletal ultrasound. Measurements were undertaken using “ACUSON Antares (Siemens, Erlangen, Germany)” with a multifrequency linear probe, between 7.27 and 11.43 MHz. For each patient, the examiner recorded the length, width and thickness of both patellar tendons.
During measuring, patients were placed in a supine position, with 30° knee flexion to avoid eventual length differences. Patellar tendon length was defined as the distance between the most proximal point of the anterior tibial tubercle and the most distal point of the patella. Width and thickness were calculated 2 mm inferior from distal patella and at 2 mm superior to tibial insertion. Mean of both values was recorded. Additionally, each measure was repeated three times.
Rehabilitation protocolAll patients followed the same rehabilitation program and follow-up schedule with the same surgeon. After the surgery, the knee was immobilised with 2 plaster splints. At day 2, drainages were removed and the knee was discharged for 1 week. After the first week, splints were removed and passive knee mobilizations were allowed. At week 4, patients started progressing in weight bearing and strength exercises as tolerated. Pool exercises were allowed at week 6, outdoor cycling at month 3 and progressive running at month 4. Unrestricted sport activities started at month 6.
Statistical analysisA descriptive analysis of the evolution of the patellar tendon size was performed using descriptive statistics, mean and standard deviation. Paired t tests were used to compare patellar tendon size between injured and uninjured limb and between pre-op and post-op values. Statistically significant values were set up at a p value of < 0.05.
EthicsThis study was accepted by the ethics committee of the same private facilities where the study was conducted. All subjects consented their participation on the study. All procedures in this study were conducted according to the statements of the Declaration of Helsinki and their posterior revisions (Fortaleza Brasil, 2013).
Results43 subjects were enrolled in the study. However, one patient was excluded for missing the follow-up appointments due to a change of residence. A final sample of 42 subjects were included in the study. Sample characteristics data is available in Table 1.
Sample characteristics.
| Mean | SD | |
|---|---|---|
| Male | 35 (83,3%)* | |
| Age | 31,67 | 7,00 |
| IMC | 25,11 | 3,19 |
| Tegner Pre | 6,71 | 0,74 |
Patellar tendon length, width and thickness was assessed in both legs before the surgery and at 1, 2, 4, 6, 9 and 12 months after the surgery. US assessment data is presented in Table 2.
Patellar tendon size evolution of the injured and uninjured limbs. Mean (SD).
| Month | Length | Width | Thickness | |||
|---|---|---|---|---|---|---|
| Injured | Uninjured | Injured | Uninjured | Injured | Uninjured | |
| Pre-op | 46.69 (6.11) | 46.71 (6.21) | 30.12 (3.53) | 30.20 (4.23) | 3.58 (0.54) | 3.73 (0.74) |
| 1 | 48.26 (6.38) | 46.39 (5.37)* | 33.68 (4.37) § | 30.24 (4.90)* | 5.43 (1.23) § | 3.67 (0.51)* |
| 2 | 45.76 (6.06) | 45.34 (5.57) | 32.94 (3.91) § | 28.92 (3.36)*§ | 5.81 (1.39) § | 3.66 (0.58)* |
| 4 | 45.15 (5.79) | 44.94 (5.35)§ | 32.73 (3.56) § | 29.63 (3.14)* | 5.38 (1.66) § | 3.58 (0.52)* |
| 6 | 44.42 (6.18)§ | 44.79 (5.33)§ | 31.42 (3.29) § | 29.64 (3.65)* | 4.89 (1.53) § | 3.55 (0.62)* |
| 9 | 43.21 (5.72) § | 44.47 (5.25)§ | 30.61 (3.06) | 29.10 (3.39)* | 4.40 (1.08) § | 3.70 (0.61)* |
| 12 | 43.23 (5.94) § | 44.25 (5.23)§ | 30.16 (3.07) | 28.98 (3.28)*§ | 4.29 (1.09) § | 3.73 (0.55)* |
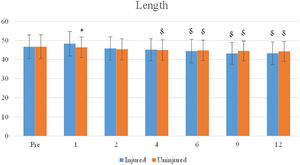
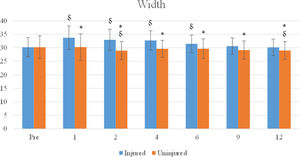
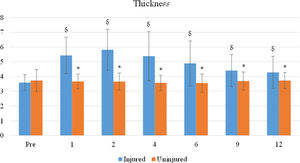
No differences were observed in pre-op values between injured and uninjured limbs (p > 0.05). The evolution of patellar tendon size of both legs is shown on Figs. 1–3.
Patellar tendon length of the injured limb showed a significant increase (from 46.69 mm at pre-op to 48.26 mm at the first month post-op) (See Fig. 1). Then, it decreased progressively until stabilizing at 43.23 mm at 12-months post-op (p < 0.05). Length of the uninjured patellar tendon followed the same decreasing tendency reaching 44.25 mm at 12-months post-op. Differences between both patellar tendon lengths were only found at 1-month post-op (p < 0.05) due to the increase in tendon length of the injured limb.
A significant increase on patellar tendon width was observed at 1-month post-op (p < 0.05). After first month, the width decreased progressively until returning to pre-op values at 9-month post-op (Fig. 2). The uninjured limb showed more stable tendon width values, with only a significant decrease at 2-months post-op. Differences between both legs were significant from 1-month post-op until last follow-up at 12-month post-op.
Regarding tendon thickness, the injured leg showed a significant increase from pre-op values until 2-months post-op (p < 0.05), when it started a progressive decrease (Fig. 3). However, at 12-months post-op tendon thickness was significantly higher than pre-op values (p < 0.05). Patellar tendon thickness of the uninjured leg remained stable during all the follow-up period (p > 0.05). The between-leg comparison revealed significant differences from the 1-month post-op until the 12-months post-op, due to the increase in tendon thickness of the injured leg.
DiscussionThe principal finding of this study is the significant changes in the affected patellar tendon size after BPTB-ACLR in comparison with pre-op values and the contralateral unaffected limb.
Patellar tendon length showed a significant decrease from 1-month post-op until final follow-up at 12-months post-op. At the end of the study, the patellar tendon was 3.46 mm shorter that pre-op values. The evolution of the patellar tendon length after BPTB-ALCR has been previously described.17 In a recent study from our group involving the same cohort, the use of patellar tendon in ACLR did not modify the patellar height within the radiological follow-up at two years after surgery.18 Kartus et al. observed similar results. They studied the MRI changes of a group of patients two years after BPTB-ACLR and described no differences between patellar tendon length, thickness and width between subjects with and without donor-site problems.7
The disagreement between those findings with the current results could be explained by the assessment method. While radiographic and MRI studies are the most commonly reported measurements for the evaluation of the patellar tendon length, several authors have suggested ultrasonography as a valid alternative.19 Seijas et al. showed that US measurements of the patellar tendon were comparable to anatomical measurements obtained intraoperatively.15 On the other hand, Ciloglu et al. studied the sonographic changes on patellar tendon length after tibial osteotomies, reporting a positive correlation between sonographic measurements and functional outcomes.20
Another explanation for the discrepancy between previous results and the current study could be the follow-up time. The results presented by previous studies were evaluated two years after ACLR, while the present study has a follow-up period of 12 months. Our results showed a tendency towards stabilization of the patellar tendon shortening at the 9th month after surgery, suggesting that a normalization of the patellar tendon length could occur between the first and second year after operation. Though, further studies must evaluate the sonographic changes of the patellar tendon length in BPTB-ACLR patients with longer follow-up times.
Patellar tendon width and thickness followed a similar progression, with an initial increment in tendon size during the first 1-2 months post-operation followed by a progressive return to normal contralateral values. Those changes could be explained by the initial inflammatory phase that occur in the tendon after harvesting its central third in the BPTB-ACLR.21
Järvelä et al. described the ultrasonographic changes in the harvested patellar tendon 10 years after BPTB-ACLR.22 They reported an increased thickness of the harvested patellar tendon compared with the uninjured contralateral limb. We have observed similar results at 12 months post-operation, suggesting that those findings may last for at least 10 years after the surgery. They also observed several ultrasonographic changes, such as calcifications, hypoechoic lesions and patellar osteophytes, while none of those were observed in the contralateral healthy limb.22 These results concur with previous investigations that have related the ACL injury history with an increased prevalence of articular degenerative changes.23,24
Finally, patellar tendon from the uninjured leg showed a significant decrease in length and width at 12 months compared to preoperative values. The contralateral tendon is not involved during the surgical procedure, but it can be indirectly affected by workload modifications during the postoperative rehabilitation due to the initial weight-bearing status or its participation in bilateral rehabilitation exercises (such as squatting, quadriceps eccentric training or change of direction programmes). Further studies must focus on the influence of the rehabilitation programmes in the sonographic measures of the patellar tendon.
Some limitations must be taken into consideration when reviewing the current study. Firstly, this is a single-centre study with a limited sample size. Further studies should confirm these results in other regions with different population groups such as sedentary or athletic patients. In addition, ultrasound has some intrinsic limitations such as the examiner-dependence. In this study, a physician (MR) with more than 20 years of experience in musculoskeletal ultrasonography performed all the sonographic evaluations. Additionally, this study did not evaluate the translation of patellar tendon size changes into clinical outcomes. Further studies must focus on this relation. This study has also several strengths. Firstly, all surgical procedures were undertaken by the same medical team and the same harvesting technique was used in all subjects. Secondly, all patients followed the same rehabilitation program with the same physiotherapist team. This study will provide clinicians and practitioners with reference values of the sonographic evolution of the patellar tendon after BPTB-ACLR in soccer players, which will help them in the detection of abnormal tendon size evolutions. Further studies are needed to explore the same variables in different populations such as athletic or sedentary subjects with longer follow-up, and the influence of the changes in patellar tendon size in clinical outcomes such as pain or function.
Ethics approvalAll procedures performed in this study involving human participants were approved by the ethics committee of the Hospital Quironsalud Barcelona in accordance with the 1964 Helsinki Declaration and its later amendments (Fortaleza, Brasil 2013).
Informed consentInformed consent was obtained from all subjects enrolled in this study. Patients also signed informed consent regarding publishing their data related to this study.
Statements and financial support: No financial support has been received for the realization of the present study. This project has been conducted as part of a PhD project of the author Roberto Seijas.
The data used and described in this study has not been previously published in any national nor international journal. However, it has been exposed in the final presentation of the PhD project of the author Roberto Seijas which took place in Valencia, Spain in 2017.
The current manuscript has 2206 words after excluding title, tables and bibliography.