The World Health Organization (WHO) provides physical activity guidelines tailored to diverse populations and life stages, with an emphasis on aerobic and strength exercises. Despite endorsements from private and public institutions, the recommendations lack real personalization and fail to consider the multidimensional, dynamic, subjective and context-dependent nature of health and fitness. Drawing on recent research, this work aims to: a) review the theoretical assumptions and evidence-based research behind the WHO guidelines, b) update the guidelines on the basis of Complex Systems Science and Network Physiology, and c) reveal how to empower users/patients to transition from dependency on prescriptions to self-efficacy. The proposed exercise criteria aim to foster adherence, interoceptive awareness, self-regulation and self-responsibility towards health and fitness.
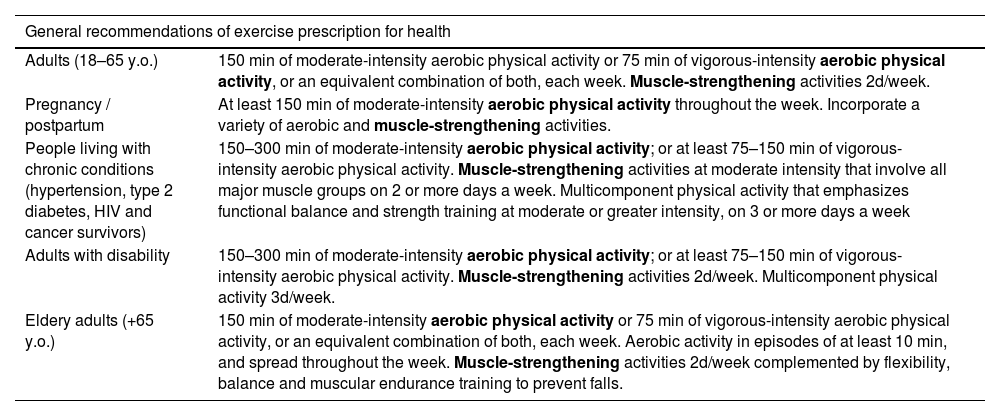
The physical activity guidelines provided by the World Health Organization (WHO)1,2 offer a framework for prescribing health-promoting exercises tailored to various country contexts (e.g.3–7) The guidelines describe the benefits of physical activity and define the specific doses recommended for different types of population, from life stages (children, teenagers, adults, pregnancy, postpartum period, elderly) to patients with diseases and pathologies (cardiovascular, respiratory, locomotor, endocrine, nervous, digestive, urinary, gynecological and psychological dysfunctions like anxiety, depression, stress or eating behavior). Curiously, all target groups share similar types of recommendations. They are primarily focused on physical conditioning, incorporating strength, aerobic endurance, flexibility, and balance training. Aerobic and strength exercises constitute the main components of the program. While stretching and warm-up exercises are also included, it is acknowledged that their benefits have yet to be proven. Table 1 shows an example of the guidelines addressed to different types of populations.
The recommended dose of exercise, based on caloric expenditure, is a minimum of 150 min of moderate physical activity (30 min of moderate physical activity (converts to 4 Metabolic Equivalents (METs)) 5 days a week) or 75 min of intense physical activity per week (20 min of vigorous physical activity (10 METs) 3 days a week), complemented by strength exercises twice a week3.
Supported by private institutions such as the American College of Sports Medicine,8,9 these guidelines have been recognized as the “gold standards” in the fitness industry. The economic interests of this industry, exemplified by initiatives like the “Sport is Medicine” campaign (https://www.exerciseismedicine.org/), exert considerable influence over the selection of fitness activities and the necessary equipment for their implementation.10 These economic interests, aligned with societal values concerning body image, foster a fitness culture predominantly centered on aesthetics, thriving within fitness centers and gyms equipped with bodybuilding machines among other technological devices. Concurrently, the industry has capitalized on the promotion of muscle strengthening and resistance training for enhanced health, resulting in substantial industry growth.11,12
Embracing the slogan “some is good, more is better,” the fitness industry aligns with WHO guidelines, advocating the idea that increased physical activity correlates with greater health benefits.5 To ensure safety in this endeavor, precise quantification is essential, achieved through the use of ergometers and monitoring systems such as sports watches, activity bracelets, and other electronic devices, which are more readily available in fitness centers.13
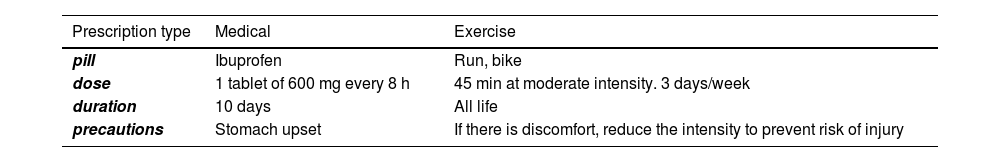
The term prescribing, used in the guidelines and meaning to order or decide on the obligation, is directly adopted from medicine. Prescribers issuing exercise in the same manner and with the same intention as clinicians prescribing a medication.14Table 2 shows the commonalities between exercise and medication prescriptions.
Commonalities between medication and exercise prescription (adapted from15).
While the effects of exercise prescription have been associated with those of prescribing medication,16 there are substantial differences between both types of treatments. Unlike drugs, which target specific molecular processes, exercise affects all body components and functions in a correlated and coordinated manner. Some authors refer to it as a real polypill, available at low cost and relatively free of adverse effects.17 In fact, its long-term and side effects differ significantly from those of medication. However, its impact is yet to be fully understood and evaluated in light of the advancements in network approaches and the introduction of connectivity measures and coordinative variables in exercise physiology.18
The adherence to the prescribed, one-size-fits-all approach of the WHO recommendations is generally limited due to a lack of real personalization and adaptability to changing personal and contextual constraints.19,20 Furthermore, taking the exercise pill without considering individual contexts (e.g., type of work, fatigue state, etc.) may increase anxiety and stress levels in healthy adults, promote exercise abandonment and increase the risk of injuries.21
These problems are further exacerbated by the rapid emergence of artificial intelligence tools like chatGPT which provide exercise recommendations for health arising from already outdated recommendations and social media influencers.22,23 However, such artificial intelligence technologies are still not recommended as a substitute for the personalized and specific exercise prescriptions provided by healthcare and fitness professionals. Moreover, the scientific evidences supporting the current exercise prescription for health have been questioned for their oversimplified assumptions and methodological limitations.24 All these reasons incite to reconsider the current exercise recommendations for health.
Our aim is to review and update the exercise guidelines outlined by the WHO, and establish criteria for attaining personalized health benefits through exercise. The ultimate aim is to transition users/patients from dependency of exercise prescriptions to self-efficacy, drawing upon recent research findings.
Updating the assumptions of the current WHO recommendationsFrom static to dynamic definitions of health and fitnessThe WHO defines health as a state of complete physical, mental and social well-being, not just the absence of disease.1 From a complex systems perspective, health is defined as a dynamic, subjective and adaptive state that emerges from the interactions between biological, emotional, social and sense-making dimensions influenced by the environment.25,26 Hence, there is no single way to promote a healthy state, and exercise should adapt to every changing context. This dynamic perspective makes exercise personalization essential to any health intervention.18
According to WHO,2 physical fitness refers to a state of well-being that allows individuals to perform daily activities with vigor and without undue fatigue. This encompasses mainly two conditional dimensions: muscular strength and endurance. This assumption does not conform with the definition of fitness in biology, where the fittest is not the strongest but the one with the greatest adaptive properties and functional diversity potentials.27,28 It is the capacity to create functional solutions to environmental challenges, known as biological intelligence,29 that enhances the possibilities of survival.28
Consequently, exercise is not simply viewed as a way to enhance physical capabilities of strength and endurance in specific contexts (fitness centers or gyms) but a way to develop a multidimensional functional diversity potential. This diversity potential is better achieved through varied, non-repetitive training stimuli.28 For example, getting up earlier to bike to work, climbing a mountain peak on the weekend or skating in the afternoons with friends are contributing to it. An exercise routine (the exercise pill), as proposed by the WHO, it is just one option which can be adequate for ‘the average’ exercise seeker.
Users: transiting from dependency to self-efficacyThe WHO recommendations of exercise prescription for health do not consider the individual personal values, goals and wishes, and overlook the specific motivations and environmental constraints of users/patients such as access to sports facilities, social support or preferred physical activities. Although prescriptions can be necessary under some specific circumstances (patients with chronic diseases, population with sedentary habits, fatigued persons), the autonomy, self-responsibility, self-regulation, self-efficacy and adherence to exercise, are better achieved through exploration, co-design and co-creation of exercise programs.21,30
Our genetics are largely shaped to support physical activity, and movement accompanies all fundamental, natural, and joyful human behavior. Consequently, exercise can be more effectively accomplished through motivating, meaningful, and adapted practices tailored to various contexts. The monotony of the exercise recommendations, sharing commonalities with medication prescriptions (see Table 2), is also a key factor to explain the lack of adherence.14,31 Even active people repeating exercises over time may reduce their motivation due to boredom.32
Fitness and health have many dimensions and can be promoted through different types of physical activities and exercise doses. In a similar way that the dose of a drug (and drug combination) is not appropriate for all patients, a universal dose of exercise (such as 150 min/week of physical activity) is not adequate for all clinical situations and personal contexts.33 For example, a sedentary person with multiple chronic conditions is still likely to significantly benefit from a small increase in physical activity, but may be harmed by too large ‘a dose’. In contrast, a working mother with three young children at home may not benefit from the same exercise prescription – her prescription needs to take account of her unique circumstance, and account for her ability to regulate the type, intensity and frequency of the exercise prescription. Like any other prescription, exercise can have harmful side effects, like causing more pain or stress in daily life. In order to regulate both physical and emotional states, subjective monitoring is crucial. Interoceptive awareness can help individuals better understand and respond to their body's signals, contributing to keep health and preventing injuries.34,35
The ‘general exercise prescription’ based on categorising the population according to disease/dysfunction or life stage arises from three ‘oversimplistic’ assumptions: a) the homogeneity of individuals in each life stage, health condition or disease category, b) the static status of diseases and personal contexts, and c) the existence of ideal health or fitness states.36
Personalization cannot be based on interindividual variabilityThe trials supporting the WHO recommendations on exercise often adhere to experimental designs founded on oversimplified assumptions and inadequate research methodologies for personalized purposes.18,37 The classification of the population by categories, pathologies or vital states do not suppose a substantial improvement of this scenario because the methodological bias is maintained.
Assuming an inexistent homogeneity among individuals, the experimental designs comparing group data means erroneously infer intraindividual variability from intergroup analyses. Indeed, research results based on population samples are not generalizable and representative of individual changes38–40 While some participants within an experimental sample may show substantial beneficial changes after an intervention, others may encounter adverse effects and others may show no response at all.40,41 However, the published literature tends to overestimate the precision of group statistical estimates and the generalizability of conclusions to individuals.42
Exercise recommendations for health should be informed by individual needs, rather than arising from entire population averages. Additionally, it is crucial to note that intraindividual variability and co-variability develop over time and, therefore, should be measured through analytical tools for time series.43 To overcome these scientific biases, some authors suggest starting by detecting individual dynamic patterns of response, afterwards clustering the common patterns, and finally generalizing them to population.44,45 That is, generalizing from individuals to population instead of from populations to individuals. Consequently, personalized recommendations should avoid reducing individuals to their dysfunctions or life stages on the basis of population average research findings because intragroup differences are huge.
Intraindividual variability includes daily, weekly, or seasonal fluctuations in vital signs like blood pressure, heart rate, or body temperature, changes in health conditions, alterations in emotional and mental states, and responses to external influences like diet, physical activity, and the environment. Considering this variability is crucial for making appropriate exercise recommendations and adapting physical activity interventions. Furthermore, as personal, social and environmental constraints change over time, the effectiveness of exercise programs tested in laboratory settings cannot be directly extrapolated to reality.44
Challenges for future guidelines editionsThe participation of users in the selection of their physical activities, instead of being mere consumers or executers of a prescribed program, is essential for their long-term adherence to an active lifestyle. To achieve sufficient autonomy and self-responsibility, educational initiatives are crucial.
When individuals realize that their health is the outcome of their interaction with the environment, and can occur both in the absence and presence of objective disease, they do not merely focus on adhering to an exercise routine. Instead, they prioritize caring for their personal and social circumstances to cultivate healthy habits that align with their inner immediate needs. Whether or not they suffer a specific disease, this shift in perspective encourages their self-responsibility towards health and exercise. For instance, they may have to change their individual perceptions of health and fitness, which often is inappropriately influenced by the media and rooted on the aesthetics and marketing industries.
Cardiovascular and strength machines, available in fitness centers, standardize body movements and restrict movement possibilities, being more likely to become monotonous.46 On the other hand, motivating and meaningful activities for the user guarantee long-term adherence47 resulting in the sustained maintenance of a healthy state.32
The interaction with professionals who are capable of transitioning from prescribing to co-designing is a key aspect of helping users/patients move from dependency to autonomy and self-efficacy. The guidelines should encourage a shift in the roles of both, professionals and users. Professionals should transition from mere prescribers to becoming co-designers and co-learners, while users should move from being passive executors to active participators in decision-making regarding their fitness and health. Exploring and creating personalized programs requires the mutual cooperation of both sides.
The involvement of the user/patient/athlete as a co-designer of the intervention is not only crucial to increase the adherence to exercise but has positive effects on mental health and the development of interoceptive awareness and autonomy in healthy adults.21 In turn, the professional educates and accompanies the practitioner to be less dependent of prescriptions. The final goal of the approach is to help them transition from dependency to self-efficacy, developing self-knowledge, self-regulation, and personal autonomy towards physical activity. The experiences of co-design show that patients and professionals can work together in a meaningful and sustainable way for both.48
Although co-designing opportunities are usually restricted to users with higher economic status and education, the exercise guidelines for health should provide general exercise and training criteria to foster pro-active, exploratory and creative behavior among users. Trusting in their ability to discover and select suitable physical activities, as well as self-regulate their doses and intensities, is essential for adherence purposes.
Practical recommendationsFrom a complex systems perspective, below are some recommendations to promote future personalized guides addressed to users, professionals, institutions and organizations responsible for physical activity and health:
- a)
To treat users/patients as multidimensional individuals and avoid reducing them solely to their pathologies or life stages,
- b)
To conceptualize fitness and health as a multidimensional and dynamic adaptive state, not reducible to physical condition, represented by strength and resistance.
- c)
To recognize the limitations of dominant scientific evidences based on experimental designs comparing group data means, and apply the results of these studies in a contextualized way.
- d)
To promote the co-design and co-adaptation of programs by adjusting them to personal and environmental conditions.
- e)
To focus on promoting the development of the functional diversity of users.
- f)
To propose motivating and meaningful activities to users, which ensure greater psychological benefits and long-term adherence.
- g)
To promote co-design and co-learning among professionals to foster their development.
- h)
To offer exercise and training criteria instead of standardized exercise prescriptions, which shift users from dependency to autonomy and self-efficacy.
- i)
To emphasize the use of subjective monitoring for developing users interoceptive awareness, self-knowledge and self-responsibility, aiming to optimize the intervention results while simultaneously reducing risks and adverse events.
- -
Health and fitness are multidimensional, dynamic, subjective and context-dependent states.
- -
Personalized exercise recommendations should avoid reducing individuals to their dysfunctions or life stages because intragroup differences are huge.
- -
Exercise criteria, instead of exercise prescriptions, empower users/patients towards self-responsibility, self-regulation and exercise adherence.
- -
Health care and fitness professionals transitioning from prescribing to co-designing help users/patients moving from dependency to autonomy and self-efficacy.
This work was supported by the National Institute of Physical Education of Catalonia (INEFC), Generalitat de Catalunya.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
To the researchers, sports professionals and volunteers who have collaborated to the “Network Physiology of Exercise: Prescribe or Co-design” project.