Flossband application in rehabilitation and sports medicine has been demonstrated to increase flexibility, improve muscle strength, dampen pain, and reduce inflammation. However, scarce evidence has presented the latent mechanisms that explain the beneficial effects of Flossband application. To fill the knowledge gap about the Flossband wrapping mechanisms and Flossband application mastering, an initial theoretical framework delineating the advantages of Flossband application mechanisms is needed. Therefore, based on the current evidence, this paper aims to summarize the potential mechanisms of the Flossband application benefits. The primary speculated mechanisms, “Pain Gate”, “Fascia Glide”, “Sponge Effect”, “Soft Tissue Ischemia”, and “Joint Effect” were proposed to illustrate how Flossband application works on soft tissues or joints to reduce pain, release fascia tension, improve muscle flexibility, decrease inflammation, and enhance muscle activation. The benefits derived from the Flossband application may be more effectively elucidated through the interaction of the five primary mechanisms mentioned above, whether applied to soft tissues or joints rather than relying on a singular mechanism. This consideration acknowledges the complexity and interactivity inherent in the Flossband application.
Fascia is a continuous connective tissue, forming a three-dimensional network that covers all the organs in the human body, such as bones, muscles, nerves, vessels and visceral organs.1 Fascia comprises collagen fibres, elastic fibres, reticular fibres and ground substance.2 Various mechanoreceptors exist in the fascia that respond to the different stimulations; for instance, Ruffini corpuscles, Pacini corpuscles and free nerve endings were found not only in the superficial fascia but also in the deep fascia, and these mechanoreceptors respond to the steady stretch, pressure, vibration, and change of ambient temperature.3 From the histological finding, fascia contains rich blood vessels and nerves, especially in the deep layer4. These specific fascia structures determine their functions of supporting, dividing, protecting, force transmission, affecting metabolism and influencing information communication.1,5 Hyaluronic acid (HA), a polysaccharide found in connective tissue and a component of the ground substances, withstands compression, provides lubrication and hydration, and plays an essential role in facilitating fascia gliding, reducing fascia viscosity, and aiding in accurate information transmission.6 The speculation evidence showed that abnormal fascia tension might alter the tension structure of collagen fibres and the composition of the extracellular matrix from a biological perspective.7 For example, fascia adhesion may disrupt the function of HA, which restricts fascia gliding, affects force distribution, and alters receptors’ pain responses.8 Additionally, abnormal fascia tension may cause increased nerve pressure and traction, raising the likelihood of nerve swelling in the affected area. This may restrict blood supply and reduce metabolism due to increased endoneurial fluid pressure.9 Furthermore, long-term fascia adhesion may result in cumulative musculoskeletal injuries, decreased mobility, increased stiffness, inhibited neuromuscular control, and stimulated nociceptor sensitization, potentially forming a vicious cycle of injury.10 To break the vicious cycles, several myofascial release approaches have been developed, and the tissue flossing technique by applying Flossband around the soft tissues or joints is one of those methods to address fascia dysfunction.
Tissue flossing using the Flossband is usually combined with passive treatments and active movements to address pain, flexibility restriction, and neuromuscular disorders. Thus, it has increasingly been used in sports and rehabilitation by practitioners for the last decade. Flossband (SanctbandTM Comprefloss, Malaysia) is a natural rubber band that is more than one millimetre thick and is applied to different soft tissues or joints by users.11 The current literature review revealed no conclusive evidence about the precursor of Flossband. In the year of 2013, Kelly Starret, an American physiotherapist and CrossFit coach, developed a new tool called flossing to accelerate recovery, improve muscle strength and increase range of motion.12 Two years later, Kelly Starret and Cordoza Glen published the book, “Becoming a Supple Leopard: The Ultimate Guide to Resolving Pain, Preventing Injury, and Optimizing Athletic Performance”, first incorporated the Flossband application, which expands a new approach to manage pain, improve sports performance as well as prevent injuries.13 In the year of 2017, Seven Kruse, a German sports physiotherapist, further expanded the Flossband application by adding the understanding of fascia in sports rehabilitation and fitness training in his book “Easy Flossing”,14 which accelerated its popularity worldwide.
Flossband application on the soft tissues or peripheral joints has been approved to manage pain, reduce inflammation, decrease myofascial tightness, increase the range of motion, activate the muscle, and improve muscle strength.11,15,16 For example, two minutes of Flossband application around the knee joint with pressure 182mmHg (±38mmHg) significantly decreased the pain intensity of the knee pain patients with a one-time treatment, compared to a control group without Flossband application.17 After two minutes of Flossband wrapping on the elbow, combined with the elbow flexion and extension movements, significantly reduced pain around the elbow.18 Furthermore, four weeks of Flossband combined with sports therapy significantly reduced ankle joint inflammation for the patients with acute ankle sprain compared to the group with sports therapy only.19 Additionally, the Flossband wrapped on the thigh combined with the passive muscle twisting and active knee flexion movement significantly improved the straight leg flexibility compared to the control group.20 Moreover, two minutes of Flossband wrapped on the gastrocnemius, with pressure 160mmHg (±3mmHg), combined with dynamic stretch significantly improved the calf muscle force development,21 and wrapping the Flossband on the thigh with pressure 154.3mmHg (±13.3mmHg), combined with dynamic squat significantly improved the maximum isometric voluntary contraction.22 Although the mechanisms underpinning the beneficial effects of Flossband application are not fully understood, few hypotheses about these mechanisms were postulated. A theoretical framework connecting the advantages of Flossband application mechanisms is needed to fill in the knowledge gap about the Flossband wrapping mechanisms and Flossband application mastering. Therefore, this paper aims to summarize the potential mechanisms of the effects of Flossband application based on the currently available evidence.
The potential mechanisms of Flossband ApplicationSeveral speculations on the potential mechanisms of Flossband application benefits, for instance, the theory of “Pain Gate”, “Fascia Glide”, “Sponge Effect”, “Soft Tissue Ischemia” and “Joint Effect”, were listed below:
Mechanism of “Pain Gate”The “Pain Gate” mechanism is one of the speculated explanations for the benefits of Flossband application on soft tissues or joints to reduce pain. This theory, proposed by Wall and Melzack,23 suggests that pain perception can be modulated by the opening or closing of the nerve gate located in the dorsal horn of the spinal cord. This modulation occurs through the activity of small diameter C-fibers and Aδ-fibers or larger diameter Aβ-fibers. Non-painful stimuli, such as compression, skin rubbing, or temperature changes, may activate Aβ-fibers, which may, in turn, activate inhibitory neurons. In the animal model, these inhibitory neurons may close the gate in the spinal cord, thereby reducing the perception of pain by inhibiting the transmission of pain signals from C-fibers and Aδ-fibers.24 Flossband, as a compression tool, exerts pressure on the skin, which may activate large diameter Aβ-fibers, thereby reducing pain. This activation of Aβ-fibers could be one factor explaining the pain reduction observed after Flossband application. Sympathetic activities closely related to pain perception and their excitability may exacerbate the pain perception.25 However, various mechanoreceptors, like Ruffini and Pacinian corpuscles, are present in the skin or the fascia layers. These mechanoreceptors play a role in inhibiting sympathetic nervous system activity when stimulated.26 The sympathetic nervous system is responsible for the ‘fight or flight’ response, which includes increasing heart rate, constricting blood vessels, regulating muscle relaxation response, and others.27,28 When mechanoreceptors are activated, they can induce a parasympathetic response, promoting relaxation and reducing stress-related physiological responses. Although no study has yet examined the effect of Flossband application on mechanoreceptor activation, it is thought the Flossband compression on the skin may stimulate these mechanoreceptors, leading to the inhibition of sympathetic activity. Additionally, the compression may restrict the blood flow, which may produce analgesic effects through releasing beta-endorphins, and the endorphins may influence the speed of pain signal transmission to the brain, which may lead to improved brain response to the pain.29
It is worth noting that the mechanism of Flossband application for pain management may be associated with Aβ-fiber activation, sympathetic activities, and beta-endorphin release. However, current evidence is insufficient to confirm these associations. Therefore, future research is needed to elucidate the exact mechanisms of Flossband application from these perspectives.
Mechanism of “Fascial Glide”“Fascia Glide”, as the second speculated mechanism, explains the benefits of Flossband application on the soft tissues to release the fascia tension, improve muscle flexibility and reduce pain. The assumption of Flossband wrapping on the soft tissue combined with the exercises produces the cohesion force (downwards) and twist force (lateral to medial or media to lateral). These combined forces form shear force (opposite the wrapping direction) acting on the myofascial. Firstly, the shearing force may help the fascia slide between each layer, decreasing myofascial tightness, which is the main effect of improving muscle flexibility after Flossband application.30 Secondly, Flossband compression on the soft tissue increases the intramuscular pressure and may increase myofascial friction during muscle contraction, improving the deep soft tissue temperature. Previous evidence showed that improving the thermal effects of deep soft tissue decreased the fascia viscoelasticity,31 which may also explain the benefits of the soft tissue extensibility after wrapping Flossband. Thirdly, shearing force may reshape the fascia by changing the HA status. HA with a gel status may cause densification of the fascia, which may relate to fascia layers not moving independently,32 and this fascia glide restriction may affect abnormal proprioception responses, such as pain sensitization.33 However, Flossband application on soft tissue may help improve muscle flexibility and reduce pain by restoring fascia function, remodelling the HA status, and reducing receptor sensitization through fascia glide, as speculated by the “Fascia Glide” theory. It is worth noticing that further high-level evidence is needed to investigate these effects.
Mechanism of “Sponge Effect”“Sponge Effect” is the third speculated mechanism explaining the benefits of applying a Flossband. What is the “Sponge Effect”? In general, the “Sponge Effect” refers to the alteration of fluid flow, such as blood flow, lymph flow, ion flow and extracellular flow, through Flossband compression and release. Specifically, the "Sponge Effect" occurs when the Flossband compresses soft tissues by wrapping from the distal to the proximal limb region, squeezing blood flow toward the heart. Upon releasing the Flossband, fresh blood gradually returns to the compressed area, accelerating blood metabolism.34 The “Sponge Effect” also impacts fascia hydration. Cole35 revealed that fascia extrudes water when compressed, which affects the fascia's water content. During the stretching of soft tissue, fascia hydration decreases, and upon release, the fluid content rehydrates to the initial level or even beyond.36 Flossband compression may temporarily dehydrate the fascia, which rehydrates after the compression is released. This dehydration and rehydration cycle helps maintain fascia health and function. However, Flossband compression may also increase the viscosity of the extracellular matrix through HA aggregation, which can lead to soft tissue stiffness and dysfunction.37 Releasing the Flossband promotes rehydration, reducing stiffness and restoring tissue function. Improved fascia hydration reduces adhesions, enhances fascia gliding, aids in force distribution, and alters receptor responses to pain.8 Furthermore, the “Sponge Effect” suggests that Flossband application may affect lymphatic drainage. Flossband application on the soft tissue induces the compression of the superficial fascia, which may reduce the space of the fascial network, leading to lymph vessel compression.38 Upon releasing the Flossband, lymph flow restores gradually, following the “low-resistance pathway” of connective tissue fibers, accelerating interstitial fluid movement, including water, ions, and small solutes. This process may help reduce tissue inflammation by promoting efficient lymphatic drainage.39 Oedema or inflammation occurs due to fluid accumulation in the body's interstitial spaces. Various factors, including increased vascular permeability, increased vascular pressure, lymphatic return obstruction, and others, can cause this accumulation.40 Flossband application as compression therapy may diminish inflammatory responses by decreasing fluid influx and promoting lymphatic drainage, which may reduce swelling and oedema. Vogrin et al.41 hypothesized that Flossband application diminished inflammatory responses by reducing inflammation influx. Even though the speculated mechanisms of the "Sponge Effect" explain how Flossband wrapping benefits soft tissue by reducing inflammation and oedema, improving fluid dynamics, and enhancing flexibility, further high-level evidence is needed to understand how Flossband application affects inflammation and oedema.
Mechanism of “Soft Tissue Ischemia”“Soft Tissue Ischemia”, as the fourth of the speculated mechanisms, explains the benefit of Flossband application on the soft tissues to improve muscle contraction. The mechanism of tissue flossing involved with Flossband application may be associated with soft tissue ischemia. Pavlů et al.34 demenstrated that the blood flow significantly decreased after two minutes of wrapping Flossband on the upper arm compared to the other side without Flossband application. Driller et al.42 pointed out that wrapping the Flossband with 178mmHg compression for around two minutes on the soft tissue may cause blood flow restriction or local blood occlusion. Based on the previous evidence, applying around 110mmHg compression on the proximal end of the forearm induced vascular occlusion,43 160mmHg compression on the upper limb moderately restricts moderate blood flow, and 300mmHg compression on the upper limb leads to full blood occlusion.44 Flossband wrapped in soft tissue were proven to produce blood flow restriction with venous occlusion, and temporary soft tissue ischemia may theoretically stimulate various physiological and biochemical responses in the human body, such as recruiting fast fibres, increasing the secretion of growth hormone (GH) and norepinephrine (NE), activating neuronal nitric oxide synthase (nNOS), and increasing protein synthesis,45 which may contribute to enhance the strength. In a word, while the theoretical basis for the benefits of Flossband compression exists, further research is essential to validate these effects and understand the specific hemodynamic and physiological changes associated with its use.
Flossband compression on the blood vessels reduces blood flow, which leads to a reduction in oxygen supply. This supply causes lactate to accumulate in the plasma, resulting in metabolite buildup and the recruitment of slow-twitch fibres.34,46 Meanwhile, the metabolite accumulation may stimulate sympathetic nerve activity through chemoreceptive reflex mediated by intramuscular mechanoreceptors and group III and IV afferent fibres.47 The type of III and IV afferent fibres help the fast-twitched fibres recruitment, which increases muscle contraction capacity. Moreover, some evidence showed that lactate accumulation in the intramuscular environment plays a crucial role in regulating the secretion of GH and NE,48 and increasing the GH and NE may contribute to muscle mass and size.49 Increasing the GH may stimulate the synthesis and secretion of insulin-like growth factor 1 (IGF-1), and IGF-1, as a growth mediator, fastens cell fusion and contributes to muscle hypertrophy.50 Flossband application through compression and release, the restricted blood vessels return to reperfusion and the increased flux of Ca2+;51 On the one hand, Ca2+ release generates the contraction of cross-bridge, and on the other hand, Ca2+ release activates the nNOS. nNOS activation increases the NO release, which further triggers the release of hepatocyte growth factor (HGF) from the muscle extracellular matrix, then HGF co-localized with c-MET receptor on the satellite cells, which helps the cell re-fusion.52 In addition, some evidence reported that blood flow occlusion leads to cell swelling, which may contribute to muscle growth by promoting mTOR signalling.53 Even though the mechanism of blood occlusion inducing the production of the Reactive Oxygen Species (ROS) remains controversial. Some evidence reported that blood flow occlusion increases ROS production, which increases muscle glucose intake.54 Therefore, Flossband application on the soft tissues may produce the subsequent hormone regulation and metabolic responses, which may help explain muscle strength increase after Flossband application.
Mechanism of “Joint Effect”“Joint Effect” is the fifth of the speculated mechanisms explaining the benefits of applying a Flossband on the peripheral joint, such as decreasing pain, reducing inflammation and improving joint mobility. What is a “Joint Effect”? “Joint Effect” hypothesizes that Flossband compression on the joint produces a cohesion force, alters intra-articular fluid pressure (IAP), and redistributes synovial fluid within the joint cavity. Evidence shows that IAP plays an essential role, and it is closely related to active or passive joint movements, particularly at the end range of joint flexion or extension.55 Rutherford56 demonstrated that the effect of IAP depends on whether active muscles distract or compress the knee joint capsule. Flossband wrapping on the joint provides pressure around the joint combined with active and passive movements, which may increase intra-articular pressure, and help retain the vital lubricating synovial fluid in the joint. This can potentially provide a larger joint space, improving the sliding surface between the muscles and joints.57 Ultrasound evidence suggests that applying external compression around the knee could increase joint space associated with fluid shifting and synovial fluid volume.58 When the synovial fluid returns to the synovial cavity, the joint space may widen, possibly explaining the range of motion after Flossband application. Additionally, evidence indicates that removing large effusions from the joint cavity can temporarily relieve pain,59 which may explain the pain reduction observed after Flossband use. The “Joint Effect” speculation primarily shows that Flossband application around the joint may help return the synovial fluid to the joint cavity, which may increase the joint space, decrease inflammatory responses, and reduce pain. However, it is essential to note that these effects are based on hypothesized mechanisms and initial evidence. Therefore, further research is essential to validate the “Joint Effect” and comprehensively understand the impact of the Flossband application on joint function and pain management.
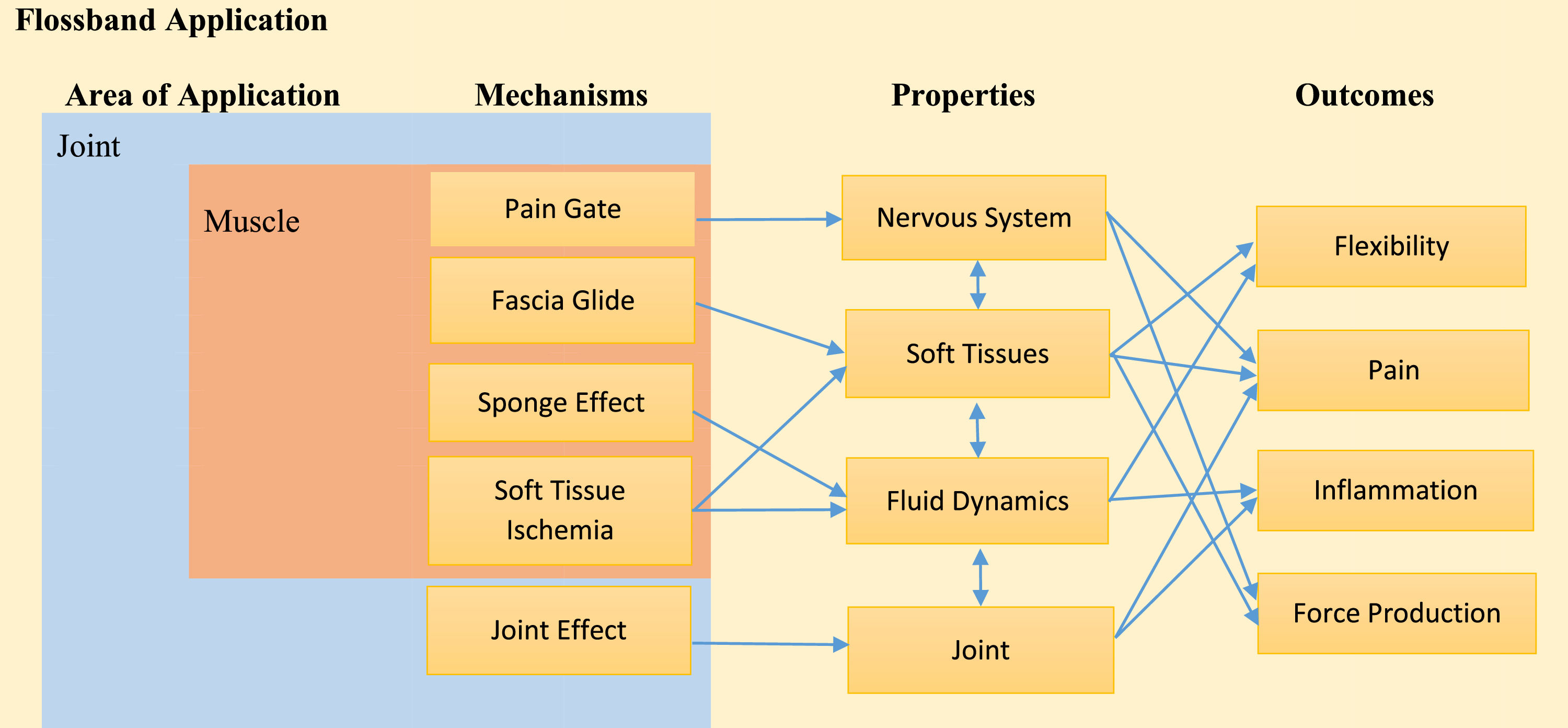
Theoretical frameworkFig. 1 presents a theoretical framework outlining the potential mechanisms of applying Flossband to various body parts. The Flossband is primarily used on joints and muscles, leading to positive outcomes such as increased flexibility, reduced pain, decreased inflammation and improved muscle force production. These benefits are mainly associated with five hypothesized mechanisms, including “Pain Gate”, “Fascia Glide”, “Sponge Effect”, “Soft Tissue Ischemia”, and “Joint Effect”. Different mechanisms are proposed based on the specific body part to which the Flossband is applied. For instance, four mechanisms, including “Pain Gate”, “Fascia Glide”, “Sponge Effect”, and “Soft Tissue Ischemia”, are the primary ones used to explain the benefits of Flossband application on the muscles. However, when explaining the benefits of conducting the Flossband on the joint, the extra potential mechanism of the “Joint Effect” shall also be considered. This framework first postulated how each mechanism operates through distinct pathways to produce beneficial outcomes. For example, applying a Flossband to muscles may influence neural response regulation, modify soft tissue properties, and alter intra- and inter-vascular fluid dynamics. These changes contribute to managing pain, increasing flexibility, reducing inflammation and enhancing muscle force production. Additionally, the framework emphasizes the interdependence of these mechanisms, highlighting the complexity of interaction among multiple factors. It suggests that a comprehensive understanding of the Flossband benefits requires considering multiple mechanisms and their specific pathways. Further research is essential to validate these mechanisms and elucidate their precise roles in achieving the observed therapeutic effects of the Flossband application.
ConclusionThe primary speculated mechanisms behind the Flossband application include “Pain Gate”, “Fascia Glide”, “Sponge Effect”, “Soft Tissue Ischemia” and “Joint Effect”. These mechanisms help explain the benefits of Flossband use, such as reducing inflammation, decreasing pain, improving flexibility and enhancing muscle strength. However, due to the complexity and interactivity of these mechanisms, the benefits derived from the Flossband application are likely better understood through the combined interaction of multiple mechanisms.
Future perspectiveThis is the first paper to summarize the potential mechanisms behind the benefits of the Flossband application, potentially contributing valuable insights to the field by enhancing our understanding of its various mechanisms. However, it is worth noticing that the benefits of Flossband application on different soft tissues or joints still require further investigation. In particular, studies should focus on the micro-level details of the biomechanical responses of the human body during and after Flossband application. This includes examining changes in hormonal levels, the intracellular and extracellular environment, fascia hydration status, blood metabolism, and pain-related substances.
All authors declare no conflict of interest.