There is little information regarding the acute repercussions of anterior cruciate ligament (ACL) reconstruction on muscle activation, especially on the proximal hip muscles. Thus, this study analyzed the acute effects of ACL reconstruction with doubled semitendinosus/gracilis (ST/G) autografts on lower limb muscle activation. Fourteen male recreational athletes that presented a primary unilateral ACL rupture and underwent the ACL reconstruction with an ST/G graft. Surface electromyographic (sEMG) signal were recorded from each participant during the maximal voluntary isometric contraction (MVIC) of the gluteus maximus and gluteus medius, vastus lateralis and vastus medialis, semitendinosus, biceps femoris, and medial gastrocnemius muscles and also during bipodal mini-squatting with open and closed eyes, before surgery and 15 days postoperatively. (sEMG) signal were normalized to isometric peak electromyography.
The postoperative assessment showed reduced muscle activation in the gluteus maximus (p = 0.013, d:0.48) in non-operated limb and also in the muscle gluteus medius (p = 0.013, d:0.79), vastus medialis (p = 0.035, d:0.63) semitendinosus (p = 0.001, d:2.46), biceps femoris (p<0.001, d:1.5), and medial gastrocnemius (p = 0.001, d:1.45) during MVIC in the operated limb. The postoperative assessment also revealed alterations in the sEMG activity of the hip and local thigh muscles in the operated and non-operated limbs during mini-squatting with opened eyes and closed eyes (p<0.05). ACL reconstruction surgery with a doubled ST/G autograft may promote immediate changes in lower limb muscle activation of the operated and non-operated limb.
The anterior cruciate ligament (ACL) plays an essential role in knee biomechanics, acting as a primary stabilizer against anterior tibial translation in relation to the femur, and with a secondary role in restricting medial knee rotation.1 In addition, it has been demonstrated that ACL promotes protection of the joint cartilage and meniscus, thus reducing the possibility of joint degeneration.2
ACL rupture has become increasingly common in high-performance sports. It has been reported that 70% of ACL injuries occur under non-contact conditions, that is, as a result of an altered movement,3 for example, when an athlete is trying to decelerate and changes the direction of movement with the foot fixed on the ground, or when excessive knee valgus and medial or lateral rotation stress in the knee occur without any contact with another athlete causing the ACL rupture.4 Thus, biomechanical changes that cause excessive knee valgus can become a dangerous condition for injuries to this joint.5 Other factors, including bone anatomy, neuromuscular control, hormonal regulation, and genetics, are known to contribute to ACL injury when the lesion results from a non-contact event.6
In a prospective study,7 it was observed that the hip abductor and lateral rotator muscles were weaker at the beginning of the season in athletes who sustained and ACL injury. The authors also concluded that athletes who presented a force ratio of less than 20.3% of body weight for lateral rotators and 34.4% for hip abductors were at increased risk of ACL injury. These findings are reinforced by the concept that the increased risk of ACL injury is multifactorial and requires a set of biomechanical and neuromuscular changes, acting simultaneously, which may vary depending on the movement performed, for example, jumps or squats.8 In this context, the weakness of the hip abductors and lateral rotators,2,8 the excessive hip medial rotation mobility, and the restriction of dorsiflexion,9 alone or in combination with athletic movements, have been highlighted.
ACL reconstruction restores the mechanical stability of the knee joint, but altered movement patterns are common after surgery, which is why many athletes cannot return to the level of ACL pre-injury function.10 In this sense, with reduced proprioception or afferent articular response of the knee, a disturbance in the neuromuscular control may occur and affect the motor responses, resulting in sensorimotor dysfunction of the injured limb.11 Although the main objective of ACL reconstruction is to restore the patient to his/her level of pre-injury activity, there is evidence that changes in the function of the quadriceps, hamstrings, and gluteal muscles remain, even after an athlete returns to his/her level of pre-injury activity.12,13
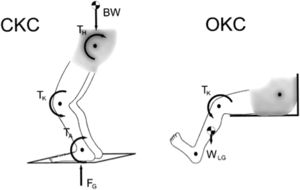
From a clinical point of view, another critical aspect is that previous studies have only analyzed muscle activation in the late postoperative period of ACL reconstruction (Hansen et al., 2017; Vairo et al., 2008).13,14 There is strong evidence that patients undergoing ACL reconstruction have a faster recovery when using rehabilitation protocols that combine open kinetic chain (OKC) and closed kinetic chain (CKC) (Fig. 1) exercises in comparison to protocols using only CKC activities,15 without causing major stress in the ligament and at the patellofemoral joint.16
In addition, it is known that rehabilitation should focus on strengthening exercises as well as exercises that enable a patient to regain dynamic stability of the knee and return to pre-injury activity level.17 The approach to factors that may lead an individual to future injury, such as weakness of the hip muscles, should also be part of rehabilitation.
To our knowledge, no study that analyzed muscle activation in the immediate postoperative period of ACL reconstruction has been found in the literature. In this way, a proposal that investigates the immediate repercussions of the reconstruction on the lower limb muscular activation is innovative and relevant to clinical practice, since it enlarges clinicians’ knowledge about the neuromuscular deficits already present at the beginning of rehabilitation. Thus, physiotherapists need to be aware of changes in movement patterns as well as in neuromuscular performance that could be present in patients undergoing ACL reconstruction in order to elaborate specific protocols to minimize possible recurrence of the lesion and to avoid chondral degeneration at the knee joint.
In addition, it is important to identify possible specific neuromuscular changes in the operated limb and also in the non-operated limb, which is the purpose of the present study, both in quadriceps muscles18 and in muscles that acting on the hip,19 already in the acute phase after ACL reconstruction. Such changes are potentially modifiable through interventions, during the rehabilitation, optimizing the entire process.20,21 Thus, this study aimed to investigate the immediate or acute effects of ACL reconstruction on lower limb muscle activation. It was hypothesized that ligament reconstruction has immediate impacts on muscle function, not only in the local thigh muscles, but also in the hip proximal muscles.
MethodsStudy design and sampleThe prospective study was designed to analyze the acute effects of ACL reconstruction with doubled semitendinosus/gracilis (ST/G) autografts on lower limb muscle activation. Fourteen male recreational soccer athletes (mean ± SD; age, 31.31 ± 9.66 years; height, 1.75 ± 0.06 m; body mass, 79.65 ± 12.57 kg; body mass index, 25.96 ± 3.76 kg/m2; injury time 17.5 ± 0.70 months) participated in this study. A recreational athlete was defined as anyone participating in aerobic or athletic activity at least 3 times per week for a minimum of 30 min per session,22 which reached level 5 in the Tegner activity scale.23 To be included in the study, the participants had to also present a primary unilateral ACL rupture verified by arthroscopic or magnetic resonance imaging, clinically diagnosed by a positive signal in the Lachman or anterior drawer tests and not have performed preoperative rehabilitation, in order to standardize the sensorimotor conditions for the baseline assessment, among the different participants. The ACL reconstruction was performed by the same orthopedic surgeon, with the graft obtained always injured leg. The participants underwent the same rehabilitation protocol after surgery: the first 2 weeks, with a focus on controlling of swelling or pain, regain full extension (without post-op brace) and gradually increase knee flexion, gradually increase weight bearing and thereby normalize the gait (without crutches).
The exclusion criteria were: any men with a current injury or a previous surgery in the lower limb, or who had cardiovascular, pulmonary, neurological, or systematic conditions that limited physical activity.24 All the study participants read and signed an informed consent form before the assessments, and all testing procedures were approved by the University's Ethical Committee (process n. x.xxx.xxx/xxxx).
ProceduresAfter the physical exam, a surface electromyographic (sEMG) assessment of the gluteus maximus and gluteus medius, vastus lateralis and vastus medialis, semitendinosus, biceps femoris, and medial gastrocnemius muscles was carried out during maximal voluntary isometric contraction (MVIC), following pain tolerance levels (score on visual analogue scale until 3) and during a bipodal mini-squatting task in different demands (with open and closed eyes), before surgery and 15 days postoperatively. The sEMG data were obtained using a Trigno 8 Channel Wireless acquisition system (Delsys, Inc. Natick, MA, USA). The signal acquisition mode was sampled at a frequency of 1000 Hz. The sEMG system had a common mode rejection of 90 dB, an input impedance of 1 MΩ, and gain set to 1000.
The electrodes were adhered in the muscles to the operated and non-operated limbs following the SENIAM guidelines (http://www.seniam.org/) while ensuring that the electrodes were placed in-line with the estimated resting pennation angles so that the same muscle fibers intersected both electrodes. Prior to electrode application, the corresponding areas were shaved and gently abraded with fine-grain sandpaper to remove any hair or debris, and the abraded areas were cleansed using alcohol wipes.25 The same template was used in relation to the positioning of the electrodes in the pre and postoperative period, guiding the second evaluation, through previous reliability study.
The MVIC data were collected during the manual muscle strength test in which the joint position was standardized, as follows: gluteus medius (20° of hip abduction in side-lying) and gluteus maximus (5° of hip extension in prone position with knee flexion at 90°),26 vastus lateralis and vastus medialis (60° of knee flexion in seated position),27 semitendinosus and biceps femoris (45° of knee flexion in prone position), and medial gastrocnemius (neutral position of the tibio-tarsal joint in supine position).28 Five EMG signals for each muscle group were acquired during the MVIC test for each participant. Each maximum contraction was performed for 6 s, with a 2-minute interval between contractions.
At the end of the sEMG assessment, all of the participants underwent a dynamic and simultaneous assessment of all muscle groups while performing a bipodal mini-squat. With the participants positioned in orthostatism, maintaining a base of 10 cm distance between the midline of each calcaneus and with the upper limbs positioned along the body, they were asked to stare at a point located at eye level, 2 m away. From this position, they were asked to perform the mini-squat task until they reached 30° of knee flexion, with safety, and returned to the initial position, performing the entire movement during the 6-second period, during which the sEMG activity was recorded. Five sEMG acquisitions were recorded with the participants performing the task in the opened-eyes condition and 5 additional sEMG acquisitions were recorded with the participants performing the task in the closed-eyes condition. The same assessment protocol was applied to all participants, with the aim of assessing neuromuscular conditions and performance. Prior to testing, all volunteers were familiarized with the test and the knee flexion amplitude (30° of flexion), controlled by a specific motion analysis software - Visual3D v5.02.07 (C-motion Inc. Rockville, USA).
Outcome measuresRaw data were smoothed in the EMGworks Acquisition software 4.3 (Delsys, Inc. Natick, MA, USA) using a high pass and a low pass Butterworth digital filter with a cut-off frequency of 20 Hz and 500 Hz, respectively; a notch filter (60 Hz) was used to control electrical interferences. To analyze the muscle activation, Root Mean Square (RMS) and peak of muscle activation data were processed, excluding the first and last seconds of EMG, totaling 4 s. EMG data were normalized to MVIC, allowing the evaluation of the activity level of the muscle during the task under investigation in relation to the maximum neural activation capacity of the muscle.
Statistical analysesAll statistical analyses were performed using Statistica™ software (version 7.0, StatSoft, Inc, Tulsa, OK, USA). First, descriptive values (means, standard deviations) for each variable were obtained. The data were analyzed with respect to their statistical distribution and variance homogeneity using the Shapiro-Wilk W test and Levene's test, respectively. With respect to the parametric data, Student's t-test for dependent samples was used to intragroup comparisons (pre- X post-reconstruction) for each limb. With respect to the non-parametric data, the Wilcoxon signed-rank test was used for intragroup comparisons. Bonferroni correction was used in the setting of multiple comparisons, to correct the experiment-wise error rate when using ‘t' tests in multiple comparisons (with Bonferroni correction, p-value<0.0166 was accepted as significant). The effect size (ES) was calculated using Cohen's d by the G* Power 3.1.7 software.
ResultsThe MVIC data from the initial preoperative evaluation and 15 days after ligament reconstruction are represented in Table 1. The results demonstrate that there was a significant difference between the pre- and post-reconstruction sEMG values in the non-operated limb for gluteus maximus (P = 0.013; d = 0.48) and operated limb for the gluteus medius (P = 0.013; d = 0.79), semitendinosus (P = 0.001; d = 2.46), biceps femoralis (P< 0.001; d = 1.50), and medial gastrocnemius (P = 0.001; d = 1.45) muscles; with lower values after ligament reconstruction
sEMG evaluation of MIVC (µV) of lower limb muscles of patients undergoing ACL reconstruction with ST/G autografts (n = 14), before and after (15 days) to reconstruction surgery.
GMAX = m. gluteus maximus; GMED = m. gluteus medius; VM = m. vastus medialis; VL = m. vastus lateralis; ST= m. semitendinosus; BF= m. biceps femoralis; G = m. medial gastrocnemius. *Indicates significant difference from baseline values;%= indicates percentual difference from post-reconstruction in relation to pre-reconstruction.
The sEMG assessment data from the mini-squatting with open-eyes task, normalized by the MVIC, at the initial preoperative assessment and 15 days after ligament reconstruction are shown in Table 2. The results demonstrate that there was a significant difference between the pre- and post-reconstruction values in the non-operated limb for the gluteus maximus muscle (P = 0.005; d=−0.89) with higher values in the second evaluation. For the operated limb, there were higher values in the post-reconstruction evaluation for the gluteus medius (P = 0.011; d=−0.87), semitendinosus (P = 0.002; d=−2.19), biceps femoralis (P = 0.016; d=−0.72), and medial gastrocnemius (P = 0.004; d=−1.09) muscles, and lower values for the vastus medialis muscle (P = 0.016 d = 1.20).
EMG evaluation normalized by MIVC of lower limb muscles of patients undergoing ACL reconstruction with ST/G autografts (n = 14), before and after (15 days) to reconstruction surgery, during mini-squatting with opened eyes.
GMAX = m. gluteus maximus; GMED = m. gluteus medius; VM = m. vastus medialis; VL = m. vastus lateralis; ST= m. semitendinosus; BF= m. biceps femoralis; G = m. medial gastrocnemius. *Indicates significant difference from baseline values;%= indicates percentual difference from post-reconstruction in relation to pre-reconstruction.
The sEMG assessment data for the mini-squatting with closed-eyes task, normalized by the MVIC, at the initial preoperative assessment and 15 days after ligament reconstruction are shown in Table 3. The results demonstrate that there was a significant difference between the pre- and post-reconstruction values in the non-operated limb for the gluteus maximus muscle (P = 0.005; d=−0.81) with higher values in the second evaluation. For the operated limb, there were higher values in the post-reconstruction evaluation for the gluteus medius (P = 0.0011; d=−0.89), semitendinosus (P = 0.001; d=−2.38), and medial gastrocnemius (P = 0.004; d=−1.10) muscles.
EMG evaluation normalized by MIVC of lower limb muscles of patients undergoing ACL reconstruction with ST/G autografts (n = 14), before and after (15 days) to reconstruction surgery, during mini-squatting with closed eyes.
GMAX = m. gluteus maximus; GMED = m. gluteus medius; VM = m. vastus medialis; VL = m. vastus lateralis; ST= m. semitendinosus; BF= m. biceps femoralis; G = m. medial gastrocnemius. *Indicates significant difference from baseline values;%= indicates percentual difference from post-reconstruction in relation to pre-reconstruction.
This study aimed to analyze the acute effects of ACL reconstruction on lower limb muscle activation in individuals who underwent to this surgical procedure. It was hypothesized that ligament reconstruction has immediate impacts on function of the local knee and thigh muscles, as well as in the hip proximal muscles. This hypothesis was partially supported by the sEMG analysis of the operated limbs. Although electromechanical changes have already been documented and expected during hamstring ipsilateral muscle activation after ACL reconstruction with hamstring graft, the literature has not yet shown such acute changes after 15 days of surgery. In this way, our results identifying early deficits at rehabilitation, which deserve attention.29
Postoperative sEMG changes were observed in the MVIC test both in the proximal hip muscles (gluteus medius) and in the local thigh muscles (vastus medialis, vastus lateralis, biceps femoralis). This reduced sEMG activation in the post-ACL reconstruction was a significant finding since these muscles are fundamentally important for dynamic stabilization of the knee joint.10,30 In addition, it is important to identify possible muscle weaknesses after ACL reconstruction surgery because patients may experience these alterations in all phases of post-surgical rehabilitation; moreover, these muscular asymmetries may persist for a number of years after surgery.31 Thus, it would be important to restore the patient's motor sensory pattern, including changes in muscle activation pattern, which can be found in patients who suffered,32 in order to reduce joint overload and decrease stress on the graft, can help minimize the risk of injury, including osteoarthritis of the knee and a re-rupture of the graft.
When sEMG activity is compared for the same muscle on different days in different individuals, the sEMG signal should be normalized.26 In this sense, the raw data reported in the present study were normalized. A division of the sEMG signal during the task was demonstrated by the value of the same muscle during the MVIC, thereby allowing for the evaluation of the activity level of the muscle of interest during the task under investigation in relation to the maximum neural activation capacity of the muscle. After this process, it was possible to identify the sEMG changes during the mini-squatting with open- and closed-eyes tasks. There was increased postoperative activation for the gluteus maximus and gluteus medius muscles on the non-operated limb, as well as in the gluteus medius, semitendinosus, biceps femoralis, and medial gastrocnemius muscles on the operated limb. However, there was a decrease in postoperative activation for the vastus medialis muscle on the operated limb in relation to the preoperative activation. It should be noted that the increase in normalized activation that occurred in the post-reconstruction period seems to be more significantly related to the decrease in MVIC activation (which is considered when calculating normalized muscle activation) than to the increase in muscle activation during the functional task. The decrease in MIVC in the postoperative period could be due to the protective condition in the operated limb; since protective muscle inhibition caused by the knee surgery could prevent effective muscle activation.32 In this sense, it is suggested that the data could be analyzed either in the conventional way (after the normalization procedure) or by comparing it with the original data (raw data without the normalization procedure),26 which was not done in this study.
The results of the present study show sEMG changes in muscles that are fundamentally important to knee joint ACL rehabilitation. However, these results should be interpreted with caution, and progressive evaluations during rehabilitation should be utilized in order to guide clinicians to consider the possible muscular activation deficits in each post-surgical phase. The quadriceps muscle may undergo an inhibition and atrophy after surgery for ACL reconstruction or some surgical procedure that can be performed on the knee.33 Therefore, it is crucial to identify such event and promptly intervening in it for good prognosis during rehabilitation, since both inhibition and muscular atrophy of the quadriceps and other muscles of the operated lower limb can negatively influence the neuromuscular capacity to stabilize the knee joint. In this sense, the present study identified that proximal hip muscles present alterations in muscle activation patterns in the acute postoperative moment, thus evidenced that these muscles also need an early attention, so that they can establish their activation effective, avoiding joint overloads and possible risk factors for a re-injury.
Furthermore, another study34 has shown that there are persistent impairments in the perimetry of the operated lower limb and decreased quadriceps strength in postoperative stage; these are major concerns for physiotherapists. The restoration of quadriceps muscle activation shows some evidence for the impact of persistent peripheral morphological adaptations on muscle weakness. Our results indicate that rehabilitation protocols for these patients need to address this impact in the immediate postoperative period, thus helping patients avoid secondary injuries. The tendency of protection, restriction of movement, and decrease of weight discharge in the operated limb are relevant issues when treating the lesion, and they directly influence the ability to ensure a good prognosis for rehabilitation.
In addition, we verified alterations in muscle activation of contralateral non-operated limb. This finding agreed with literature suggesting that ACL injury can influence the uninvolved limb, resulting in functional and strength deficiencies.35 Considering that the frequency of contralateral rupture after previous injury ACL may vary between 8.2 to 16% of cases36 we highlight the importance of assessing the immediate repercussions of ACL reconstruction on the uninvolved limb.
The authors recognize some limitations related to the current study. Although the mini-squatting task, seems to be a low-demand activity requiring few muscles and limited joint adjustments, our results demonstrated that there was a decrease in the activation of both the proximal hip musculature and the local knee muscles during the early postoperative period. The mini-squatting task was chosen in order not to stress the graft in the early postoperative time by a safe amplitude movement.37 However, these results must be explored in future studies in order to help clinicians better assist these patients and promote a more effective rehabilitation protocol. Identifying specific changes early, both in knee flexors and hip-acting muscles, may have important implications with respect to rehabilitation after ACL reconstruction and may thereby positively affect athletes, successful return to competition with minimal risk of re-injury. We also consider as a limitation the fact that the present study does not have an external control group, which would give us other perspectives in relation to the immediate effects of ACL reconstruction surgery. Moreover, the use of a male-only sample and the low sample size of the study, affected by the pandemic by SARS-CoV2 in our country, may be considered other fonts of limitation. Thus, these results are applicable to our participants profile, and cannot be extrapolated to other populations. Finally, another limitation is the fact that we did no measure the pain in the exam period, such the knee pain could be related to some type of movement alteration in order to protect or decrease the demand in the operated limb.38 However, despite not being objectively quantified, this sign was not perceived in any volunteers. So, we believed that the potential limiting factor of this fact is, at most, limited.
ConclusionIn conclusion, ACL reconstruction surgery with a doubled ST/G autograft may result in immediate negative changes in muscle activation of the operated and non-operated limb in individuals undergoing this surgical procedure.
The authors are grateful for the financial support obtained from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – CAPES (Finance Code 001) and Fundação de Amparo à Pesquisa do Estado de Minas Gerais - FAPEMIG (scholarship and financing – APQ 03580-13, APQ 01955-14) – Brazil; PET MEC SEsu. To the hospitals Santa Casa de Alfenas and Hospital Universitário Alzira Velano.