Femoroacetabular impingement (FAI) is a common injury in basketball, having a difficult therapeutic approach because it requires an extended period of time to be resolved once it appears. Therefore, preventing the onset of this condition seems critical in maintaining athletes’ health, and availability to compete. Because reducing training and competition volume in a professional team context is complex, the exercises presented here offer a good option for managing injured players without compromising their availability during the season. However, offseason and preseason periods are key to developing, protecting and strengthening the injured joint and its functionality for the competitive season.
At present, although injury prevention work is integrated into training sessions and an individualized physical assessment is made, injuries continue to occur because certain levels of risk are intrinsic to sports practice.1
The most frequently occurring injuries in basketball are injuries to the lower extremities,2 with increasing incidence of hip injuries in recent years.3 In the 1990s, the hip joint was identified as the cause of 3.1% of injuries,4 although in more recent studies the incidence of pathology in this joint has increased to 6.2% of injuries in NBA2; however, the coxofemoral joint has been identified in only 2% of hip injuries.4
A pathology of special interest in the hip is the femoroacetabular impingement (FAI). The pathology is determined by the existence of deformities in the hip joint that can be combined and cause impingement between the femoral neck and the anterior edge of the acetabulum, especially when there is flexion and internal rotation of the hip.5,6 Thus, 3 types of FAI5–9 are typically described: CAM, PINCER and MIXED. In the CAM type, the femoral head is oval instead of spherical or there is deformity due to thickening in the femoral neck. In the PINCER type, the edge of the acetabulum is excessively prominent in one or more areas of its circumference. In the mixed type, there is a combination of the two deformities previously described. FAI has also been described in subjects with normal anatomy, where the triggering factor of the pathology is a range of excessive mobility.5,1 CAM type deformity is the most frequent in young male athletes.5
The importance of the FAI in the young and active adult is high since it is a frequent cause of hip pain that causes joint dysfunction and that can cause labral tears in this population group.10–12 The prevalence of FAI radiological signs in the general population is estimated at between 23 and 67%13 although the existence of radiological signs does not always lead to the existence of a clinical pathology in the hip.14 However, in current studies there is evidence that FAI is more prevalent in athletes, especially in those who perform sporting movements with hip flexion, adduction and internal rotation.15,16 In basketball, this movement is frequent in the displacements with the ball, defensive movements and basket throws.
There is also consistent data that supports the idea that FAI pathology generates instability in the hip joint, and this leads to osteoarthritis developing in this joint.17
In the specific context of professional basketball, the FAI incidence does not always register “Time Loss” injuries, since they generate chronic pain that generally allows the player to continue playing for a while and it is when the joint is not adequately treated or not protected that the joint injury can be aggravated or injuries triggered in other structures due to compensation.17,18 This is also related to lower sports performance with all the consequences that this may entail for the professional athlete.
The goal of this article is to describe a conservative treatment suitable for FAI for professional basketball players, aimed at functionality and not worsening the injury, as well as for the athlete to maintain optimal sports performance during the different phases of the season.
Anatomy and biomechanics of the hipTo understand the therapeutic orientation in case of FIA, it is essential to understand the anatomy of the hip and its biomechanics. The hip joint is classified as a spheroid joint. This type of joint allows more types of movements in space.19 Thanks to its structural arrangement and the ligamentous support, the hip is a very stable joint. There are numerous muscles adjacent to the joint that are very important for balance and control of the lower limbs and spine.20–22
The joint capsule is a loose, fibrous structure that encompasses the joint. The fibers are arranged from the iliac bone toward the intertrochanteric line of the femur. There is a fibrocartilaginous labrum in the acetabulum that increases the joint surface, making it 22% larger.23 It is important to know that the labrum contains free nerve endings and sensory organs in its superficial layer that can participate in nociceptive and proprioceptive functions.24
The muscles of the anterior aspect of the hip are closely related to FAI. They are the main hip flexors: iliopsoas (psoas major and iliacus), sartorius, rectus femoris, tensor fasciae latae and pectineus. The iliopsoas has fibers that join the anterior joint capsule and intervene in the capsule's mechanical function.25 Other muscles involved in hip stability and mobility are inserted or located near the joint and include the gluteus minimus, gluteus medius, gluteus maximus, the abductor muscle group, the hamstring muscles, quadratus femoris, piriformis and gemelli.21,22
In sport, the hip is essential for the athlete's movement. Thus, in the gait and stroke biomechanics on the sagittal plane, the cyclical hip flexion and extension movement is synchronized with correct movement of the pelvis (posterior tilting during flexion and anterior tilting on the hip extension). Inadequate anterior tilting of the pelvis or a rotation at the end of the first phase of the movement can cause the athlete to excessively extend the femur, which would increase the tensile stress of the iliofemoral ligament and the anterior joint capsule.21 There is usually less mobility in the hip and pelvis on the frontal and transverse planes. Adduction/abduction movements and external/internal rotation21,26 come into play. Variations in adequate synchrony or body position can cause injuries to the hip, spine or knee.20,26
Regarding the forces acting on the hip, it must be taken into account that a male athlete can increase his body weight during the race by approximately 2.36× and in large jumps as practiced in basketball, the weight can increase approximately 5×.27 The muscles must be well trained to withstand the impact absorption due to eccentric contractions, as well as to contract hip extensors, quadriceps, hip abductors and hamstrings with force and in correct synchrony. The hip flexors are dominant during the displacement phase. The gluteus medius are very important for controlling pelvic tilt and promoting hip elevation.28 In the transverse and frontal planes, it is the external hip abductors and rotators that work eccentrically to control the movement and provide stability.20,21,28
Clinical presentation of the pathologyThe alterations in the anatomy and/or in the biomechanics of the hip are determinant for the development of FAI. The clinical manifestations are variable, although usually there is inguinal pain, pain when sitting for a long time or walking, and pain when doing sports activities that require forced hip movements, such as deep squats for example. Other times there is intermittent pain, joint blocks in the hip, a sensation of instability in the hip, etc.
DiagnosisFor an adequate and early diagnosis, it is important to recognize the symptoms of the pathology and to demonstrate the existence of skeletal alterations in the coxofemoral joint through imaging tests.29,30
The tests carried out in the physical examination include FADIR (flexion, adduction, internal rotation), FABER (flexion, abduction, external rotation), the “log roll” test (internal and external rotation of the limb with the knee in extension), the IROP test (pressure on the acetabulum in internal rotation) and the maximum squat test. The FADIR test was the most sensitive test in the physical examination for FAI diagnosis.31
For the image diagnosis, simple radiography32 magnetic resonance with or without contrast33,34 and/or the computed tomography29 are used.
TreatmentThe therapeutic options should initially be aimed at a conservative therapy establishing measures that attempt to stop progression of the injury and allow the athlete to maintain his or her professional activity at a good level. If the conservative program fails or a significant improvement is not achieved, surgical treatment should be considered.
Although surgical treatment is not the subject of this article, it is convenient to point out that the experience coincides with previous publications that indicate that the disappearance of symptoms is not always guaranteed35 the period of absence before returning to sport will be long35–38 and often forces the athlete into early retirement,35,37 However, or possibly because many more FAIs are currently being diagnosed than a few years ago, the proportion of surgical interventions is increasing with the aim of resolving the pathology.39 It is also necessary to indicate that the success of surgical techniques has risen significantly in recent years.35–37,39
Conservative treatmentAlthough conservative treatment has classically been based on sports rest, stretching and strengthening the hip and core muscles,13 what is of interest to the professional athlete is to try to manage the pathology in a manner that does not disrupt professional sports activity. Therefore, the aim is to create conservative working protocols for athletes with FAI that provide joint stability and protects against advanced joint injuries, since a relationship has been described between the degree of injury and the possible effectiveness of the treatment.13,40,41 This protocol will be designed by a transversal professional specialists team, leaded by a Sport Physician, and composed by Physiotherapist, Athletic Trainers and Strength and Conditioning Trainers.
The bases for conservative treatment should allow the athlete to maintain a complete range of mobility (ROM) without pain. And the objectives to achieve are to improve the posterior glide of the femur, strengthen the hip muscles and correct incorrect movement patterns.20
Regarding strengthening work, open kinetic chain (OKC) and closed kinetic chain (CKC) exercises must be included that activate extensors, flexors, adductors, abductors, rotators and stabilizers of the hip, as well as flexors and extensors of the knee.42 Both can be used depending on the desired speed of the movement and the amplitude of the ROM, closely related to painless mobility.43 It must be remembered that although both types of exercises increase muscle strength, CKC provides greater joint stability due to neuromuscular adaptations such as the co-contraction of other muscle groups and the response to the compressive forces generated in the joint. Also, if you work with monopodal support to control body balance, higher demand of the upper body is required, and core stability is improved.44–46 The OKC can provide greater benefits when isolating a specific muscle group. Also, in special situations, such as when the athlete has an excess body mass index, or when he/she has inadequate tolerance to physical activity and therefore cannot do CKC exercises. It is also better not to do OKC exercises when there may be a risk of falling.45,46
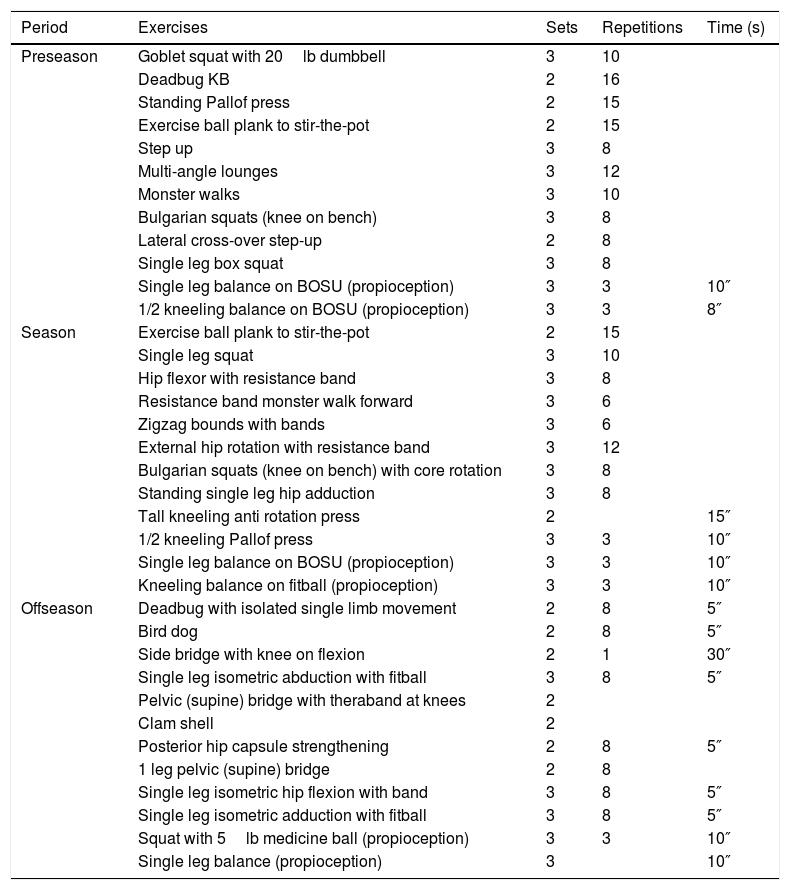
Exercise selectionBearing in mind the athlete's desire to continue to compete, the exercises prescription must be chosen according to the sport calendar and the period of the season,47 which will include “offseason” (individual after season training period), “preseason”(on team before season training period) and “during the season” (competitive period). This periodization will enable the athlete to do different exercises, or their variants, respecting the principles of adaptation, progression and variability of the loads. These exercises should be done under the premise that the athlete is asymptomatic, as well as adapting the volume and intensity of the loads required for each specific case.48 According to these premises, the protocol will be developed and supervised by the Strength Conditioning Trainer.
The proposal presented is described below (Table 1), taking into account the periodization of the exercises depending on the period of the season. Each of these phases comprises a maximum of 10 exercises, plus 2 proprioception exercises. The orientation, muscle contraction, kinetic chain, working angle are justified at the time proposed with respect to the previous work phase, as well as the posterior base.1 Painful exercises will be avoided and replaced by specific and individual adaptations. The progression to next phase will be conditioned to an asymptomatic, correct and specific functionality20 and hip muscles strength improvement.13
Conservative workouts for femoroacetabular impingement in professional basketball during the different season periods. Exercises and load according to season period.
| Period | Exercises | Sets | Repetitions | Time (s) |
|---|---|---|---|---|
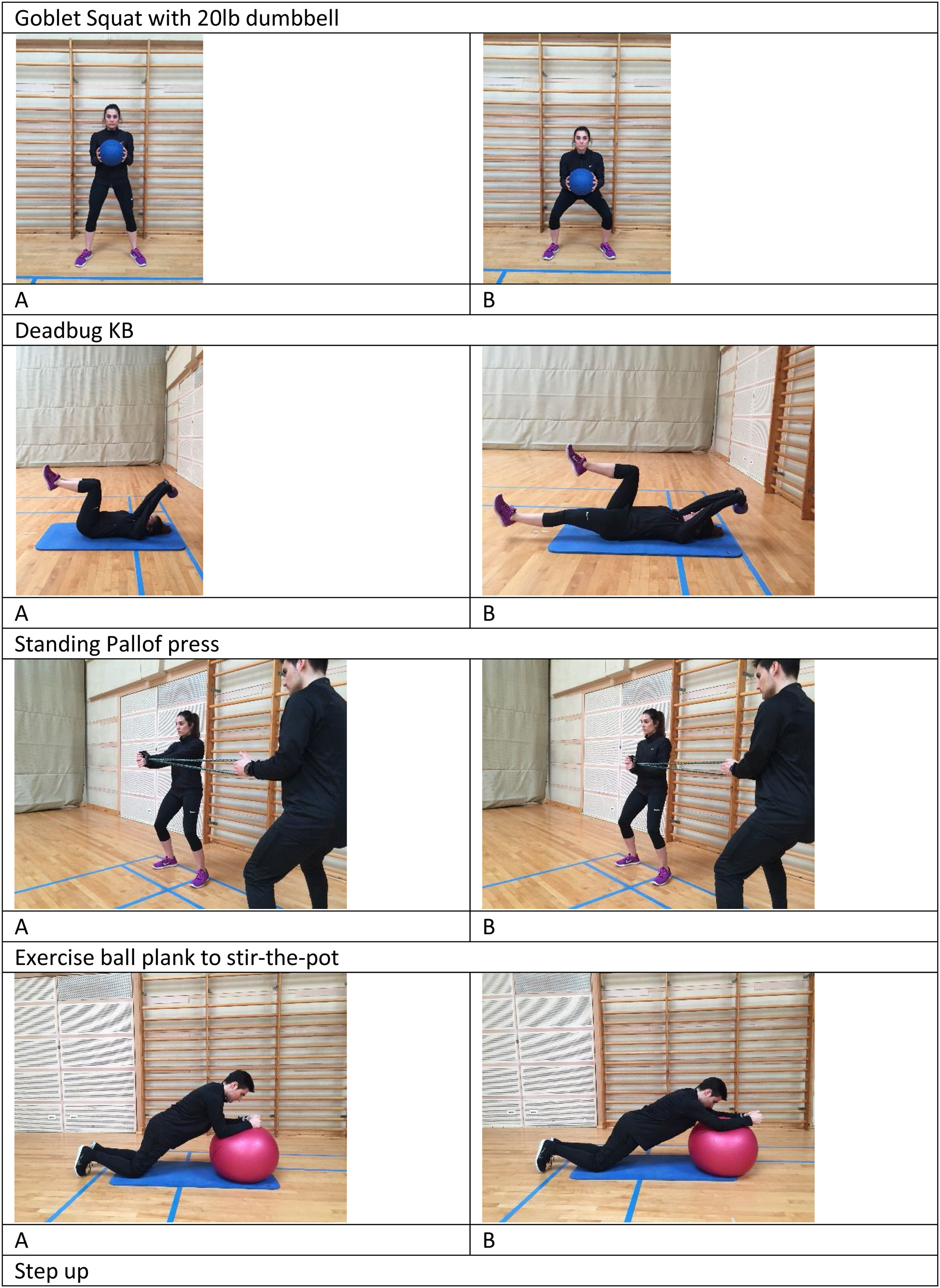
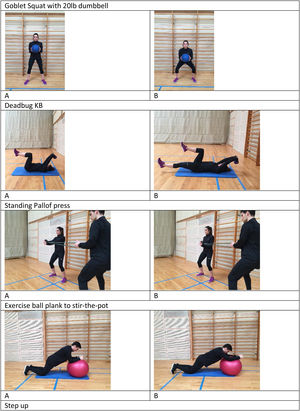
| Preseason | Goblet squat with 20lb dumbbell | 3 | 10 | |
| Deadbug KB | 2 | 16 | ||
| Standing Pallof press | 2 | 15 | ||
| Exercise ball plank to stir-the-pot | 2 | 15 | ||
| Step up | 3 | 8 | ||
| Multi-angle lounges | 3 | 12 | ||
| Monster walks | 3 | 10 | ||
| Bulgarian squats (knee on bench) | 3 | 8 | ||
| Lateral cross-over step-up | 2 | 8 | ||
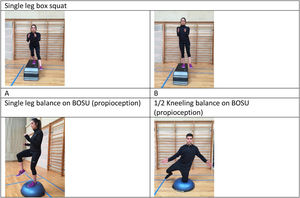
| Single leg box squat | 3 | 8 | ||
| Single leg balance on BOSU (propioception) | 3 | 3 | 10″ | |
| 1/2 kneeling balance on BOSU (propioception) | 3 | 3 | 8″ | |
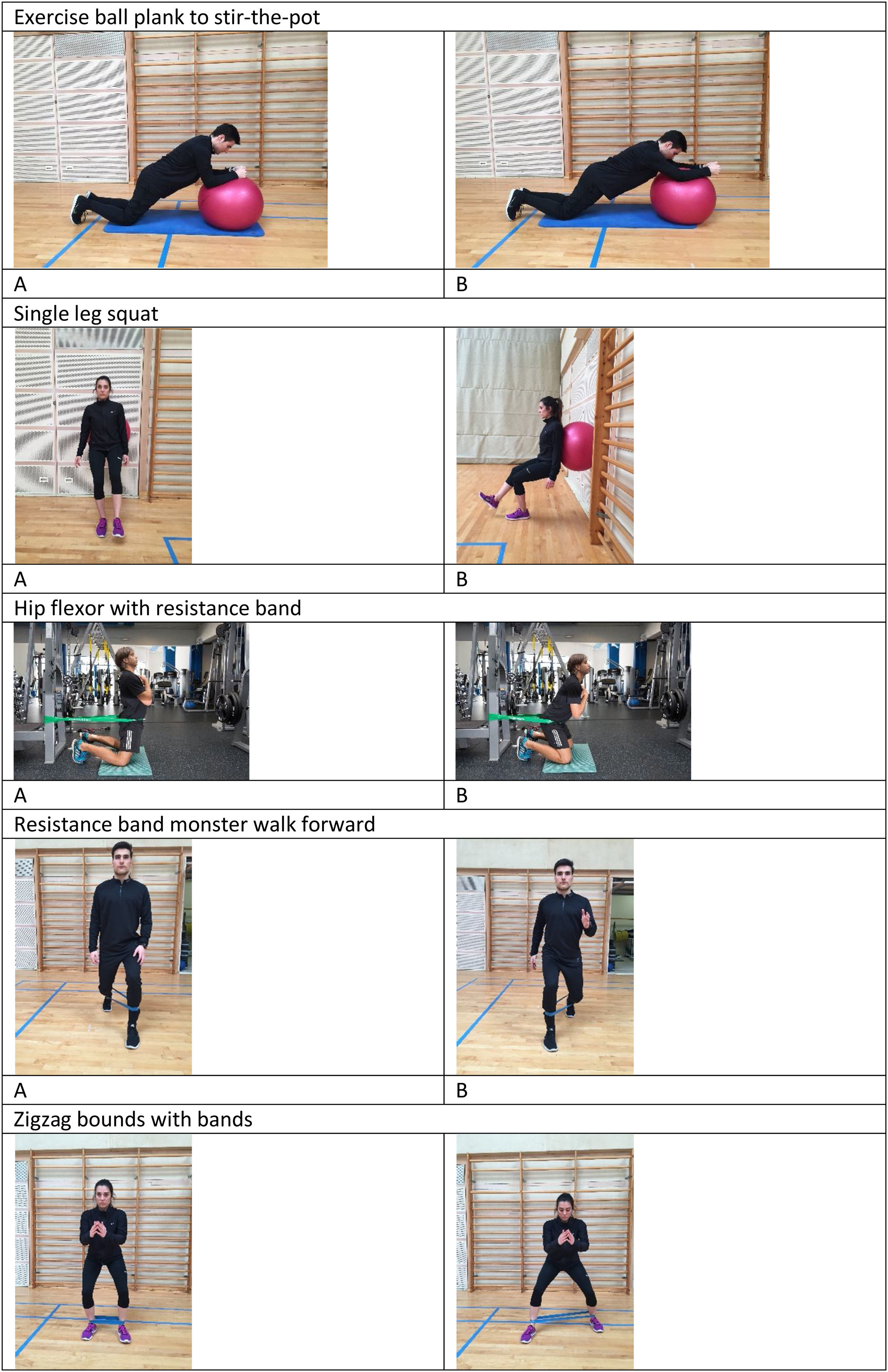
| Season | Exercise ball plank to stir-the-pot | 2 | 15 | |
| Single leg squat | 3 | 10 | ||
| Hip flexor with resistance band | 3 | 8 | ||
| Resistance band monster walk forward | 3 | 6 | ||
| Zigzag bounds with bands | 3 | 6 | ||
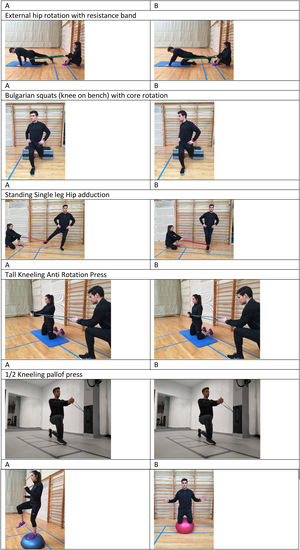
| External hip rotation with resistance band | 3 | 12 | ||
| Bulgarian squats (knee on bench) with core rotation | 3 | 8 | ||
| Standing single leg hip adduction | 3 | 8 | ||
| Tall kneeling anti rotation press | 2 | 15″ | ||
| 1/2 kneeling Pallof press | 3 | 3 | 10″ | |
| Single leg balance on BOSU (propioception) | 3 | 3 | 10″ | |
| Kneeling balance on fitball (propioception) | 3 | 3 | 10″ | |
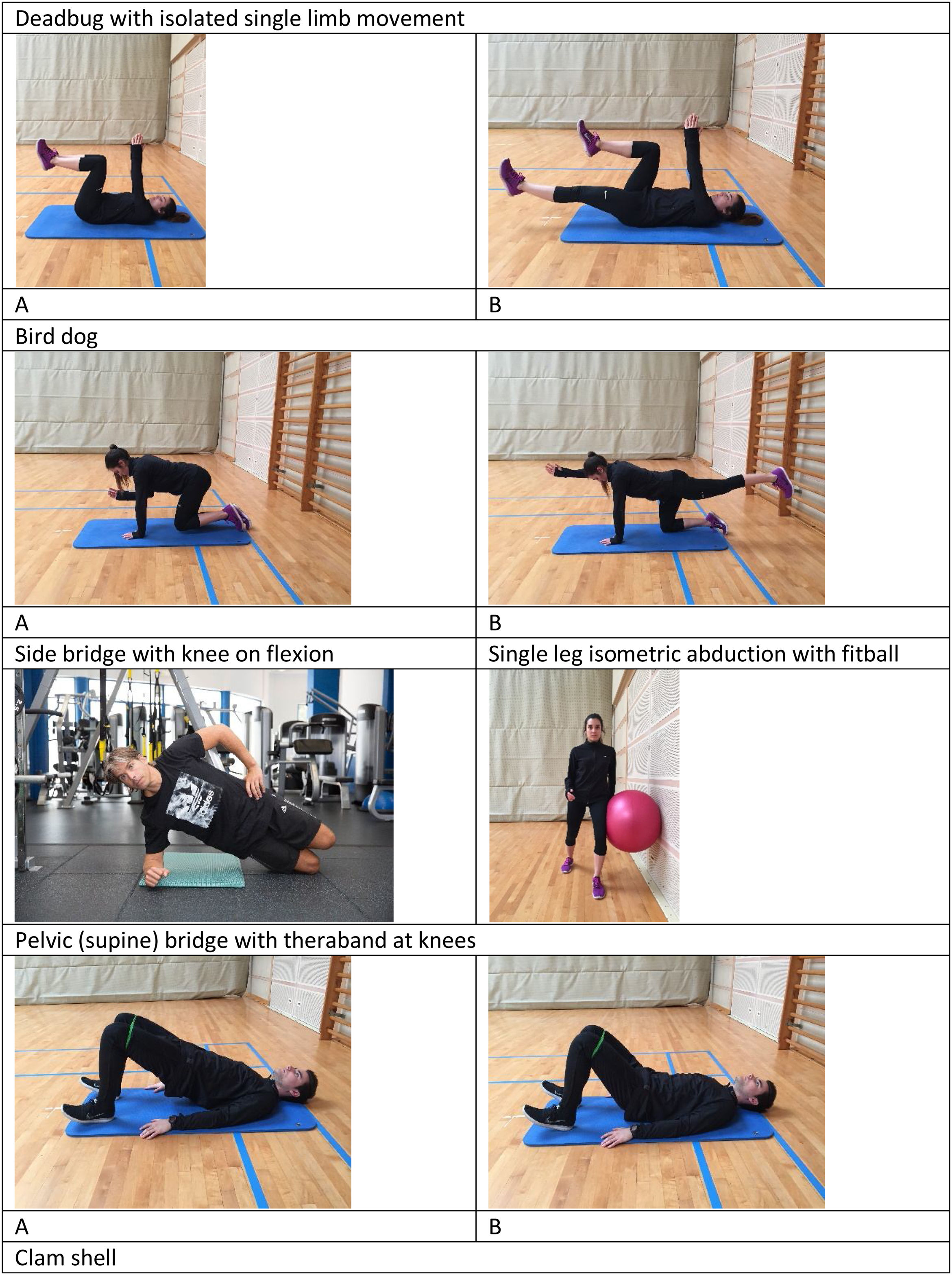
| Offseason | Deadbug with isolated single limb movement | 2 | 8 | 5″ |
| Bird dog | 2 | 8 | 5″ | |
| Side bridge with knee on flexion | 2 | 1 | 30″ | |
| Single leg isometric abduction with fitball | 3 | 8 | 5″ | |
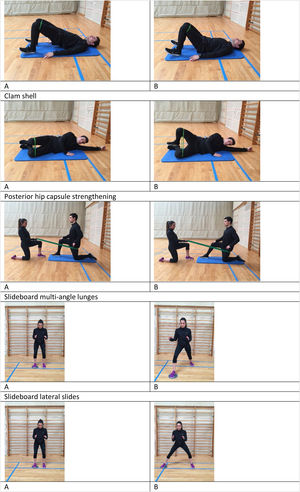
| Pelvic (supine) bridge with theraband at knees | 2 | |||
| Clam shell | 2 | |||
| Posterior hip capsule strengthening | 2 | 8 | 5″ | |
| 1 leg pelvic (supine) bridge | 2 | 8 | ||
| Single leg isometric hip flexion with band | 3 | 8 | 5″ | |
| Single leg isometric adduction with fitball | 3 | 8 | 5″ | |
| Squat with 5lb medicine ball (propioception) | 3 | 3 | 10″ | |
| Single leg balance (propioception) | 3 | 10″ |
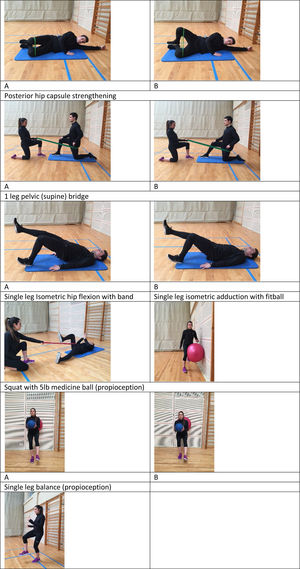
In the offseason, the aim is to correct any deficits observed during the season, reinforce the specific needs that the injury requires39,49,50 and offer the foundation for the work that will be developed in the next preseason. Therefore, more general exercises will be opted for, based mainly on isometric strength preventive work (single leg isometric hip flexion with band – resulting in improved hip flexion and with the lower glide of the femur – muscles involved: iliopsoas, sartorius, anterior rectus and pectineus; Single leg isometric adduction with fitball – improves adduction – muscles involved: pectineal and adductor magnus, longus and brevis; Single leg isometric abduction with fitball – strengthens abductors and external rotation; muscles involved: gluteus medius, tensor fasciae latae and pyramidal fascia; Squat with medicine ball – improves hip flexion; muscles involved: anterior rectus, gluteus maximus and medius and ischiosural) to be developed throughout the ROM1 (Pelvic (supine) bridge with theraband at knees – it affects hip extension, abduction and external rotation, muscles involved: gluteus maximus, ischiosural, gluteus medius, tensor fasciae latae and pyramidal; Posterior hip capsule strengthening, 1 leg pelvic (supine) bridge – improves hip extension; muscles involved: gluteus maximus and ischiosuralis – also adding multifactorial work)48 focused on the core (Deadbug with isolated single limb movement – improves lumbopelvic stability; muscles involved: transverse abdominal, multifidus, pelvic floor and iliopsoas; Bird dog – improves lumbopelvic stability and hip extension; muscles involved: erector spinae, internal and external oblique, gluteus maximus and hamstring; Side bridge with knee on flexion – improves abduction; muscles involved: gluteus medius, pyramidal, tensor fasciae latae and external oblique; Clam shell – improves external rotation and abduction; muscles involved: gluteus medius, pyramidal, tensor fasciae latae) and proprioception (Single leg balance – improves pelvic stability, muscles involved: gluteus medius and minor and tensor fasciae latae). This type of work must be carried out in the correct context: strength work while unstable can lead to certain decompensation in general,51 so prescribing this type of exercise must be subject to the absence of pain and correct functionality. The work intensities are lower than in the other periods, although the volume is comparatively high, progressing from 2 to 4 times per week (Fig. 1).
PreseasonIn the preseason period, the focus is on reinforcing the needs that the injury requires, with greater loads (in terms of volume and intensity)52 as well as more specific orientation49,53 than in the offseason (although less than the work required during the season). Protocol can be integrated on the strength workouts or as specific routine, 3 or 4 times per week. Most of the exercises are carried out in the natural sports modality position (standing) and coordinative as well as functional elements are added in the entire ROM54 (Goblet squat – improves hip flexion/extension; muscles involved: anterior rectus, adductors, gluteus maximus; Step up – improves hip flexion/extension, muscles involved: hamstrings, gluteus maximus and middle and rectus femoris; Multi-angle lounges – improves hip flexion/extension; muscles involved: gluteus maximus and medius, hamstring and rectus femoris; Lateral cross-over step up – improves hip flexion/extension, muscles involved: gluteus maximus and medius, hamstring and femoral rectus) and the different muscle contractions55 (Monster walks – improves hip abduction, muscles involved: gluteus medius, pyramidal and tensor fasciae latae; Bulgarian squats – improves hip flexion/extension and stability; muscles involved: gluteus maximus and medius, hamstring and rectus femoris; Single leg box squat – improves hip flexion/extension and stability; muscles involved: gluteus maximus and medius, hamstring and rectus femoris). The core work (Deadbug – improves lumbopelvic stability, muscles involved: transverse abdominal, multifidus, pelvic floor and iliopsoas; Standing Pallof press, Exercise ball plank to stir-the-pot – improves lumbopelvic stability, muscles involved: transverse abdominal, multifidus and pelvic floor) and proprioception (single leg balance on BOSU – improves pelvic stability; muscles involved: hamstring, rectus femoris, gluteus medius and tensor fasciae latae; 1/2 kneeling balance on BOSU – improves pelvic stability, muscles involved: hamstring, rectus femoris, gluteus maximus and medius) progressive complexity (Fig. 2).1
SeasonDuring the season, as long as the injury allows for adequate progression, the work protocol should be focused on strengthening sessions, also with a regenerative and preventive aspect.55 The work is functional and specific,47,48,53 it entails medium work volumes and intensities 1 or 2 time per week, mainly resistance (strength-resistance) (Single leg squat – improves hip flexion/extension and stability, muscles involved: gluteus maximus and medius, quadriceps and ischiosuralis; Resistance band monster walk forward – improves flexion/extension and abduction; muscles involved: gluteus maximus and medius, rectus femoris and iliopsoas; Zigzag bounds with bands – improves hip abduction and external rotation; muscles involved: Bulgarian squats (knee on bench) with core rotation – improves hip flexion/extension and stability; muscles involved: gluteus maximus and medius, hamstring and rectus femoris), as well as exercises that include the core (Exercise ball plank to stir-the-pot – improves lumbopelvic stability; muscles involved: transverse abdominal, multifidus and pelvic floor; Tall Kneeling Anti Rotation Press – improves lumbopelvic stability; muscles involved: external and internal oblique, gluteus medius and transverse abdominal; 1/2 kneeling Pallof press – improves lumbopelvic stability; muscles involved: External and internal oblique, gluteus medius and transverse abdominal) and hip mobility56 (Hip flexor with resistance band – improves hip flexion/extension, muscles involved: gluteus maximus and ischiosural; External hip rotation with resistance band – produces posterior sliding of the femur and improves external rotation; muscles involved: gluteus minimus and medius and pyramidal; Standing single leg hip adduction – improves stability of the hip; muscles involved: gluteus maximus and medius, adductor magnus, longus and brevis and pectineus). Proprioception progression is maintained (Single leg balance on BOSU – improves pelvic stability, muscles involved: hamstring, rectus femoris, gluteus medius and tensor fasciae latae; Kneeling balance on fitball – improves hip stability; muscles involved: gluteus maximus and medius, adductor magnus, longus and brevis and pectineus) (Fig. 3).
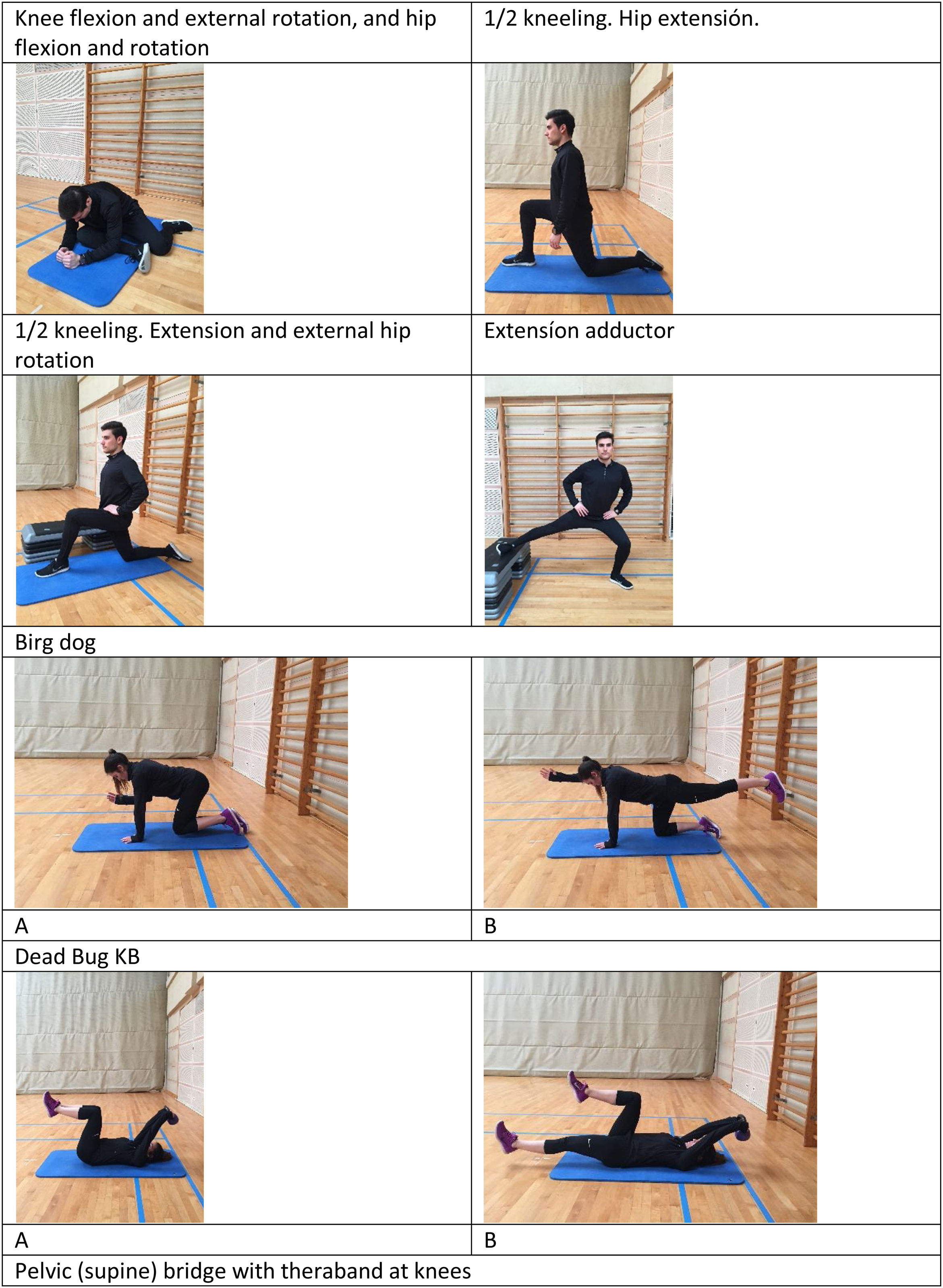
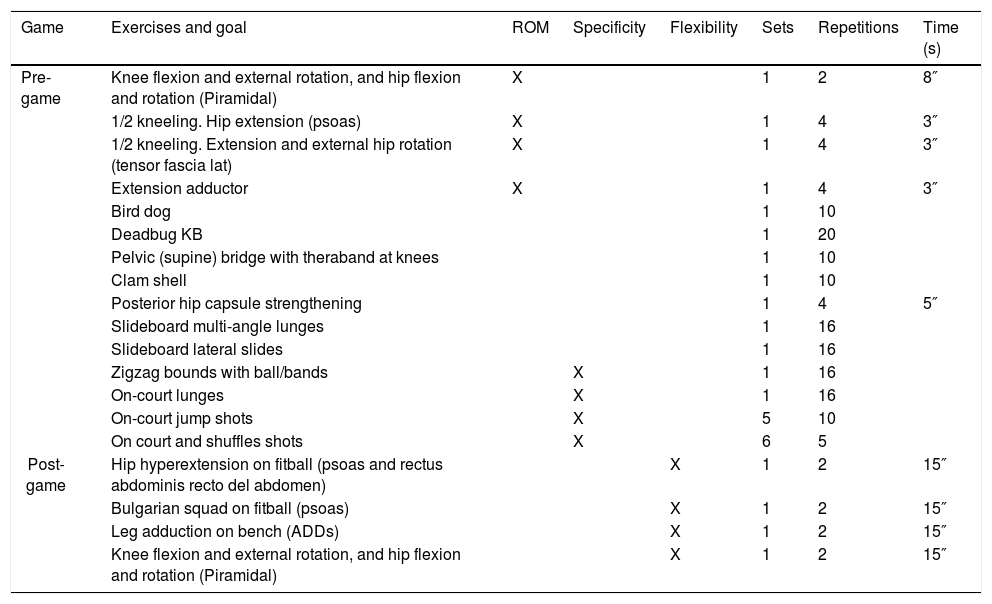
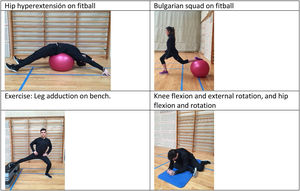
Pre-game and post-gameDuring the latter period, competitive, specific and individual workouts prior to the match (warm-up) are required, as well as post-match workouts in this case. An exercise routine is proposed before the competition begins (Table 2) based on complexity and intensity progression1,48,49,52 as well as the ROM (Knee flexion and external rotation, and hip flexion and rotation – improves external flexion and rotation of the hip, muscles involved: gluteus maximus, medius and minimus, 1/2 kneeling.Hip extension – improves hip extension; muscles involved: iliopsoas, anterior rectus, sartorius; 1/2 kneeling. Extension and external hip rotation – improves hip extension; muscles involved: iliopsoas, adductor magnus, longus and brevis; Extension adductor – improves hip abduction; muscles involved: adductor magnus, longus and brevis and pectineus). Starting with isometric contractions (Bird dog – improves lumbopelvic stability and hip extension, muscles involved: erector spinae, internal and external oblique, gluteus maximus and ischiosural; Deadbug KB – improves lumbopelvic stability; muscles involved: transversus abdominis, multifidus, pelvic floor and iliopsoas; Pelvic (supine) bridge with theraband at knees – it affects the extension, abduction and external rotation of the hip; muscles involved: gluteus maximus, hamstrings, gluteus medius, tensor fasciae latae and pyramidal; Clam shell – improves external rotation and abduction; muscles involved: gluteus medius, pyramidal, tensor fasciae latae) until it is functional (Posterior hip capsule strengthening, Slideboard multi-angle lunges – improves hip flexion/extension, muscles involved: gluteus maximus and medius, hamstring and rectus femoris; Slideboard lateral slides – improves hip abduction; muscles involved), the volume of work is low although widely varied, ending the protocol with exercises on the court with a ball (Zigzag bounds with ball/bands, On-court lunges, On-court jump shots, On court and shuffles shots) (Fig. 4).
Conservative workout for femoroacetabular impingement in professional basketball. Exercises and load for pre-game and post-game workouts.
| Game | Exercises and goal | ROM | Specificity | Flexibility | Sets | Repetitions | Time (s) |
|---|---|---|---|---|---|---|---|
| Pre-game | Knee flexion and external rotation, and hip flexion and rotation (Piramidal) | X | 1 | 2 | 8″ | ||
| 1/2 kneeling. Hip extension (psoas) | X | 1 | 4 | 3″ | |||
| 1/2 kneeling. Extension and external hip rotation (tensor fascia lat) | X | 1 | 4 | 3″ | |||
| Extension adductor | X | 1 | 4 | 3″ | |||
| Bird dog | 1 | 10 | |||||
| Deadbug KB | 1 | 20 | |||||
| Pelvic (supine) bridge with theraband at knees | 1 | 10 | |||||
| Clam shell | 1 | 10 | |||||
| Posterior hip capsule strengthening | 1 | 4 | 5″ | ||||
| Slideboard multi-angle lunges | 1 | 16 | |||||
| Slideboard lateral slides | 1 | 16 | |||||
| Zigzag bounds with ball/bands | X | 1 | 16 | ||||
| On-court lunges | X | 1 | 16 | ||||
| On-court jump shots | X | 5 | 10 | ||||
| On court and shuffles shots | X | 6 | 5 | ||||
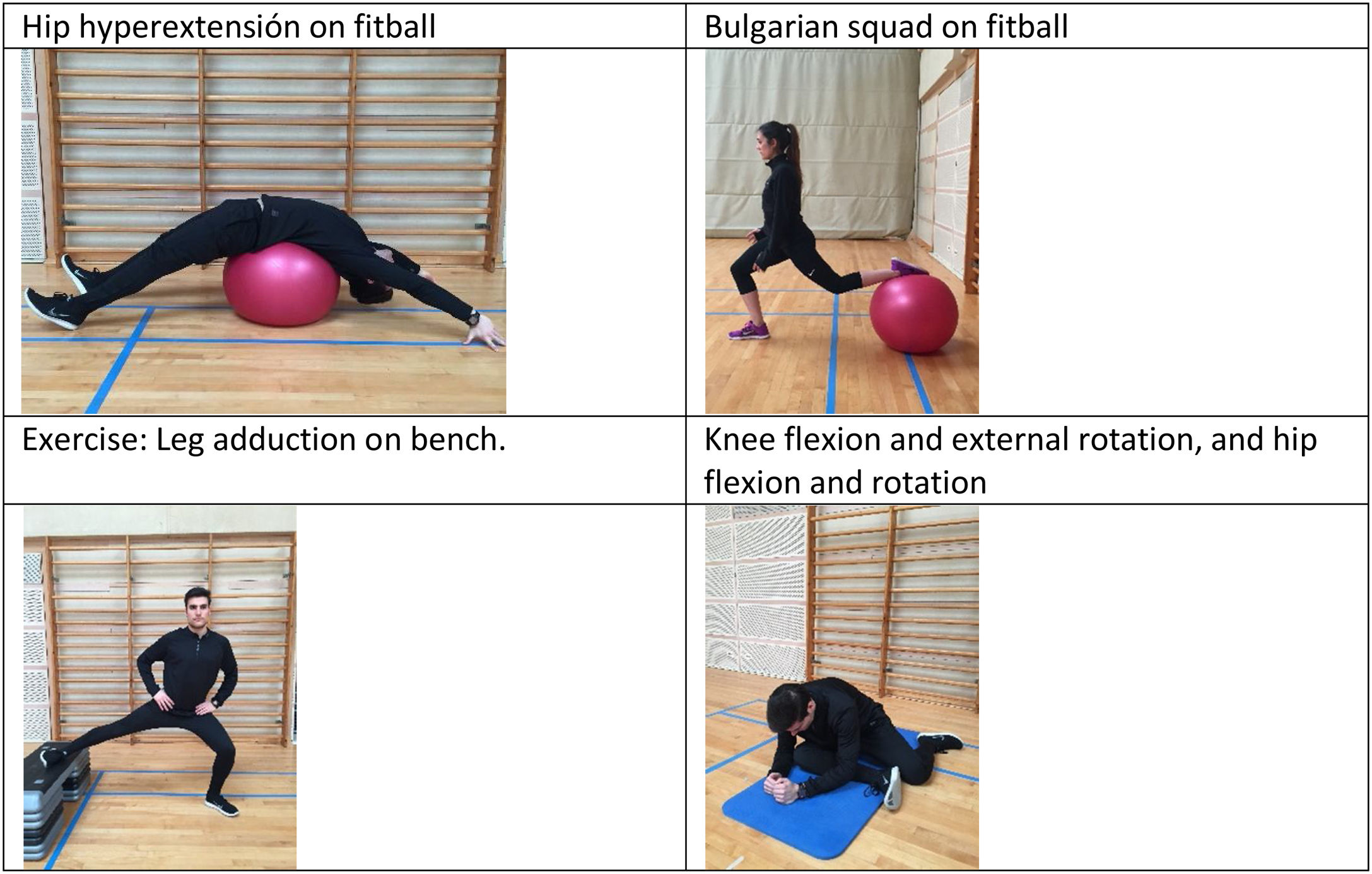
| Post-game | Hip hyperextension on fitball (psoas and rectus abdominis recto del abdomen) | X | 1 | 2 | 15″ | ||
| Bulgarian squad on fitball (psoas) | X | 1 | 2 | 15″ | |||
| Leg adduction on bench (ADDs) | X | 1 | 2 | 15″ | |||
| Knee flexion and external rotation, and hip flexion and rotation (Piramidal) | X | 1 | 2 | 15″ |
At the end of the competition, a group of four flexibility exercises are presented (Hip hyperextension on fitball – improves hip extension, muscles involved: iliopsoas, anterior rectus, sartorius and pectineus; Bulgarian squad on fitball – improves hip flexion/extension, muscles involved: gluteus maximus, hamstring and anterior rectus – Leg adduction on bench, Knee flexion and external rotation, and hip flexion and rotation – improves hip abduction, muscles involved: adductor magnus, longus and brevis and pectineus) (Fig. 5).
Practical applicationAccording to previous research, FAI is a common injury in basketball, having a difficult therapeutic approach because it requires an extended period of time to be resolved once it appears. Therefore, preventing the onset of this condition seems critical in maintaining athletes’ health, and availability to compete.1,47 Because reducing training and competition volume in a professional team contextis complex,57 the exercises presented here offer a good option for managing injured players without compromising their availability. However, offseason and preseason periods48,52 are key to developing, protecting and strengthening the injured joint and its functionality.
Although injury recovery and rehabilitation are not the main subject of this proposal, many of the exercises presented here may also be helpful for athletes recovering from FAI, adapting loads and intensities appropriately for each phase and case.
FundingNone declared.
Conflict of interestAuthors declare no conflict of interest and availability to all research data.