In the second part of this evidence- and experience-based guide, we present a progressive framework for return-to-sport following anterior cruciate ligament reconstruction in team sport athletes. This framework guides programs that return athletes to competition at maximum performance while minimizing risk of reinjury. We have built onto a framework typically used in team sports that proposes progress move from general to specific. The progression is accomplished through the use of motor learning principles and attention to hypercomplexity, which characterizes situation sports. The framework focuses on preparing players to withstand repeated high-intensity actions, combining jumps, accelerations, decelerations and changes of direction with dribbling, passing, receiving, shooting and/or reacting to their teammates and opponents while minimizing risk of reinjury.
Part I argued that return to sport (RTS) following anterior cruciate liagament reconstruction (ACL-R) requires an approach unique in team sport athletes that differs from the traditional approach. It's not enough to focus only on recovery of the injured structure(s); the injured athlete must also be prepared to withstand the demands of team sport competition. In other words, the different structures, or systems, (e.g. conditional, coordinative, emotional-volitional, creative-expressive, cognitive and socio-affective) must be readapted to sport performance in an integrated way while minimizing risk of reinjury and returning the athlete to competiton at the highest level of performance. These goals should be accomplished using basic principles of sports training, especially those of progression and individualization.
The RTS process following ACL-R can be viewed on a continuum. To structure the RTS program, Part II proposes using different levels of approach to competition that have been established.1,2Table 1 shows a generic program using approaching levels to competition for a team sport athlete following ACL-R. Initially, the rehabilitation process main objectives are biological healing of the injury and improvement and maintenance of the athlete's physical conditioning. The next phase on the continuumis return-to-training (RTT). The main objective of this phase is to prepare the athlete to tolerate group training with confidence while minimizing the risk of reinjury. The final phase of the program is return-to-competition (RTC). The main objective of this phase is to prepare the athlete for competition at maximum performance. It should also be added that once the athlete has suffered an ACL injury, it is important to address the main factors that contribute to ACL injury (e.g. hamstring strength work) to prevent re-injury throughout their career.
Objectives and criteria to progress in the return-to-sport following anterior cruciate ligament injury in team sport athletes understood as a continuum.
A flexible and specific RTS framework following ACL-R in team sports athletes is presented below, with an emphasis on the RTT and RTC phases. Although this framework focuses especially on the conditional area, the integration of all areas that influence the athlete's performance (e.g. psychological, nutritional, etc.) are still equally important.
RehabilitationAs mentioned in Part I, most team athletes who suffer anterior cruciate ligament (ACL) injury and wish to return to sport will need to undergo surgery. For this reason, the physiotherapist and the rest of the professionals who will work closely with the injured athlete during rehabilitation must have open communication with the surgeon. The surgeon will provide valuable information about aspects that will determine the treatment: type of graft, whether or not there will be meniscus repair, determination of damage to cartilage, idenfitification of associated ligamentous injuries or complications during surgery.3
ACL reconstruction surgery uses a graft to replace the ligament. The most common graft types are autografts, or grafts from the patient's own tissue (eg. patellar or hamstring tendon). Healing of the remaining patellar tendon following removal for graft occurs at approximately 8 weeks.4,5 This is faster than the healing of the remaining hamstring following removal for graft, which takes approximately 10–12 weeks. Although there is some individual variability, most authors agree that this phase can end at approximately 10–13 weeks.6,8 It should be added that the remodeling phase of the hamstring autograft is significantly longer than that of the patellar tendon (12–24 months vs 6–12 months).9 The remodeling phases for each graft type correspond with both the time the athlete is returning to competition and the time athletes are at greatest risk for a second ACL injury.10
Immediately following ACL-R, the proposed tasks will be mainly general in nature (level 0); that is, they do not transfer to sport-specific movement, but they activate fundamental movement patterns during their execution.11 The work on strength and neuromuscular control during this phase will be key during the later phases. The systematic review by Van Melick et al. (2017) on rehabilitation after ACL-R concludes that3
- -
Isometric quadriceps work is safe from the first week post-operation (level 2 of evidence).
- -
Open kinetic chain quadriceps work should be delayed until week 4 (in order to avoid elongation of the graft) and limited to 90–45° of flexion (level 2).
- -
Early bodyweight strength work does not affect posterior knee laxity (level 2).
- -
Neuromuscular training (training of the sensorimotor system in order to gain dynamic stability) should be added to strength training in order to improve knee stability (level 1).
- -
Initiating closed kinetic chain eccentric quadriceps activations 3 weeks post-ACL surgery is safe and contributes to improving quadriceps strength more than training with concentric muscular activations (level 1).
Furthermore, in this phase it is important to try to maintain the athlete's physical conditioning without jeopardizing the biological healing of the injury (eg. general metabolic-cardiovascular work or trunk strength).
Some other useful criteria found in the current literature that can be used in the decision to progress athletes to the next level include: the absence of pain (eg VAS <2–3 during walking) and edema, the restoration of the full range of motion of the knee (0–125°, full extension) and good neuromuscular control (dynamic stability) of the hip-knee-ankle complex during single leg balance (Table 2) or low-impact activities, such as walking.6,8
Useful tools and criteria recommendations to progress in specificity during the RTS post ACL-R in team sports.
| PHASE | Rehabilitation | Return to training | Return to competition | |
|---|---|---|---|---|
| Return to Activity | Return to sport | |||
| Useful criteria to move to the next phase | - Pain and edema control (e.g. VAS < 2–3 during gait)- Acceptable knee range of motion (e.g. 0–125°)- Good neuromuscular control of the trunk-hip-knee-ankle complex during activities of daily living (e.g. unilateral balance and gait) | - Good neuromuscular control (biomechanics) during FMS (e.g. Single leg squat test51) and low impact SSS (1 vs 0)- Monitoring inter-limb asymmetry (magnitude and movement strategy) in different capacities and skills:- Strength: Analytic (e.g. quadriceps, hamstrings, abductors) and fundamental movements (unilateral squat) - Dynamic balance (e.g. Star Excursion Balance test50)- Single leg jumping tests in the vertical, horizontal and lateral direction (jumping with one leg and landing with both legs52) - Running technique- Core stability (e.g. frontal and side plank31)- Acceptable ratio and co-activation between hamstrings and quadricipital muscles | - Limb alignment video analysis (biomechanics) during ACL high risk situations: - Landing Error Scoring System79 (e.g. LESS < 5) - Tuck Jump Assessment 80,81 (e.g. TJA < 6) - The cutting movement assessment score73- FMS (jumping, sprinting and CODs) and SSS successfully perform at maximum intensity, acceptable neuromuscular control and safely- Monitor magnitude (% ASI), direction and movement strategy of inter-limb asymmetries in functional tasks: - COD and agility tests (e.g. modified T-test77, COD tasks in different angles 45° /90°/180°72, reactive drills…)- Fundamental strength tasks (e.g. Bulgarian squat) or isoinertial devices skills 75 (e.g. cross step or side step)- Jump and hop tests in multiple directions76 (e.g. limb symmetry index < 90%)- Good ratio between hamstrings and quadricipital muscles8 (e.g. < 10–15%)- Fatigue resistance to intermittent and repetitive efforts, typical of team sports. Examples: - Repeated sprint ability with one or more CODs (e.g. 10* (15+15); r:30 seg75) - 30–15 Intermittent Fitness test74 | - Absence of pain or edema- Levels of strength / power and speed and quality of movement between legs similar or prior to injury (e.g. <10–15%), both in FMS and SSS- High capacity to resist high intensity repeated efforts- Good confidence and competence in technical and tactical performance- Tolerance to training / competition chronic load- Assessment of psychological readiness (e.g. ACL Return to sport after injury scale 84) |
COD = change of direction;% ASI = inter-limb asymmetry index; FMS = Fundamental movement skills; SSS = sport specific skills; RSA = Repeated sprint ability.
Finally, active work during the preoperative phase (“prehab”) is crucial to the success of the rehabilitation and the ability to return to competition following ACLR.12,13
Return-to-trainingAccording to motor learning theories, one of the best ways to learn is through imitation.14 Integrating a player with the group allows them to improve their performance by imitating their teammates. To do this, there must be a progressive increase not only in conditional and coordinative loads, but also in cognitive and emotional loads.
To describe the progression of the rehabilitation process to training, the retun-to-training period will be divided into two sub-phases: 1) Return-to-activity, and 2) Return-to-sport.
Return-to-activityAthletes in this phase usually participate actively in the rehabilitation sessions and can begin to participate in gym and track training sessions with the rest of the group, but with certain modifications or restrictions. They should avoid damaging the injured tissue or structures that surround the injured area. On a psychological level, the ability to participate in the dynamics of the group represents a great milestone for the player. On a physical level and generally, this phase focuses on improving basic motor skills through both functional strength and low-impact neuromuscular control training.
Improve strength in basic movement patternsAs this is still a time of biological healing of the injury, strength training during this part of rehabilititation is usually increased isometrically or dynamically using low loads to activate muscles and lay the groundwork for building muscular endurance (< 50% 1 RM) and strength (60–80% 1 RM) later.15 Subsequently, muscles, tendons, ligaments and cartilage should be progressively prepared to withstand the higher loads to which joints are subjected during sport-specific skills (SSS). This is known as the creation of structure (specific adapatations to imposed demands, SAID principle).16
Structure creation (SAID principle)During this phase, the creation of structural adaptations (muscles, tendons, ligaments and cartilage) through strength training becomes especially important. Practitioners should try to make strength training functional (eg. dynamic, fundamental movement) while considering the role of the neuromuscular system on active joint stabilization. As a player becomes stronger and their structure improves, they will also advance in adaptations aimed at sport movements.1 Classically, strength training with the aim to target hypertrophy is worked between 3, and 5 sets of 6–12 repetitions (per muscle group and session) and at an intensity between 65, and 85% of the one maximum repetition (1RM). As a guideline, and depending on the individual adaptations of each athlete in this phase, it is recommended to progress from lower to higher intensity and volume. Regarding the training volume, Schoenfeld and Grgic (2018) suggest that a good starting point to build hypertrophy would be to work about 10 sets per muscle group per week. This volume can be increased progressively and over time (eg. 20 weekly sets per muscle group).17 At the end of this stage athletes should be able to tolerate intensities close to 80–85% 1RM (6–8 maximum repetitions) during the fundamental strength movements of the lower limb.
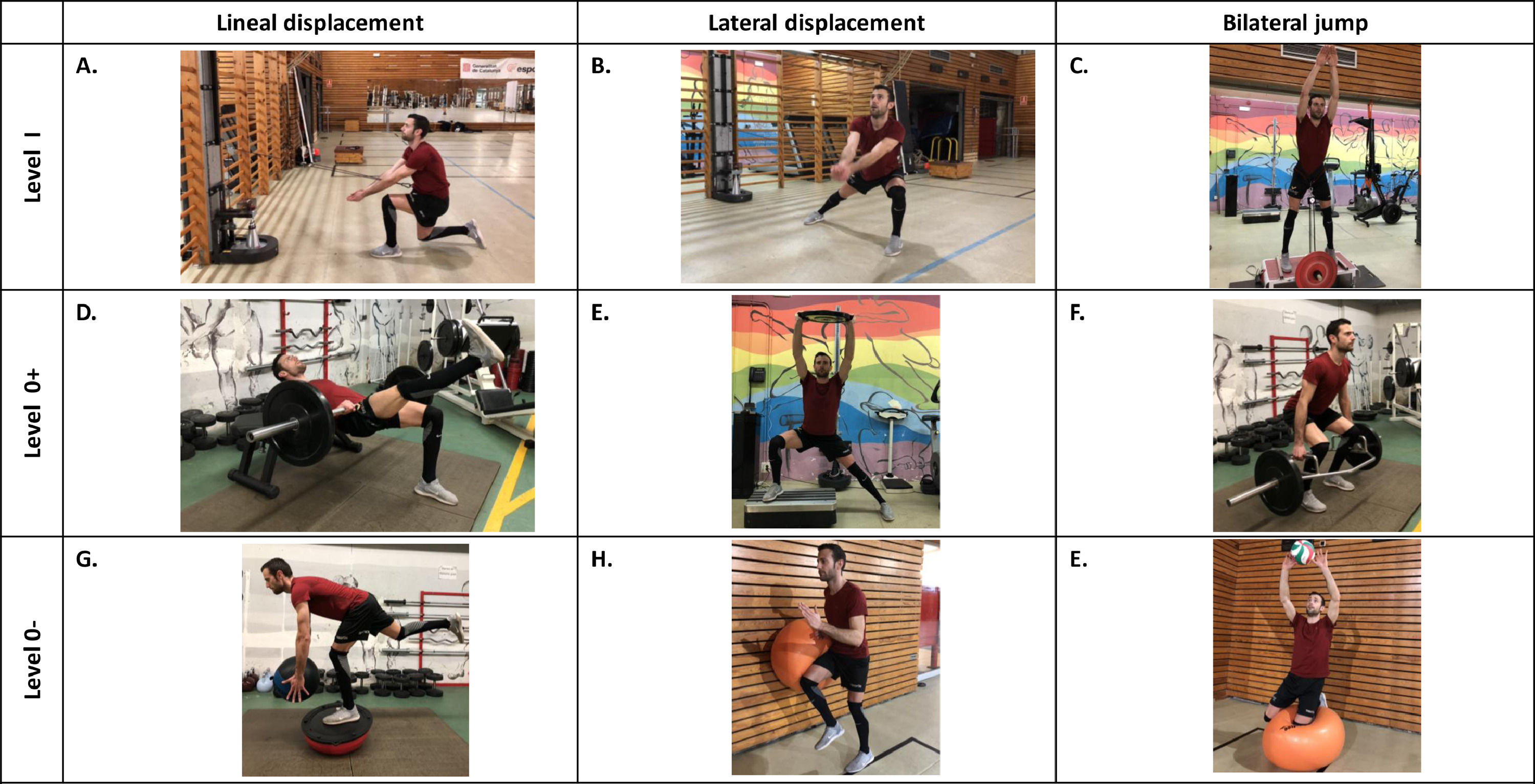
Choosing tasks (movements)At this level of progression, tasks 0+ are prioritized. The focus is on strengthening fundamental movement patterns (e.g. squat, lunge or Romanian deadlift). In the case of knee injuries, knee-dominant exercises (e.g. squat, lunge, Nordic hamstrings, etc.) and hip-dominant exercises (e.g. Romanian deadlift, glute bridge, etc.) are particularly relevant. The combination of these patterns facilitates progress toward sport-specific movements. Similar to the previous stage, it will be very important to continue focusing on the correct alignment of the hip-knee-ankle complex during triple flexion exercises of the lower limb, as well as proper trunk mechanics (Figure 1) (e.g. maintaining a slight curve in the lumbar spine during execution of a squat). Neither technique nor quality of movement should be sacrificed for the intensity of the exercise.
Tasks created to optimize low limb biomechanics (triple flexion of the hip-knee-ankle complex). This neuromuscular activation strategy improves quadriceps-hamstring coactivation and reduce dynamic knee valgus. This fact reduces joint load to which the knee is subjected during high-risk ACL injury actions (changes of direction, decelerations, and jump receptions). In addition to triple flexion of the low limb, flexion of the trunk is also important while maintaining the physiological curvature of the spine.
While limbs should be worked both bilaterally and unilaterally, unilateral tasks should be progressively prioritized because they are commonly performend in team sports. During bilateral work, it is important to emphasize limb symmetry despite the large asymmetries that are likely present. Unilateral work is key to reducing the neuromuscular asymmetry typical of the first stages of rehabilitation.18,19 During this time the injured leg will determine the load for both legs.20 In addition, unilateral work on the uninjured leg allows the athlete to take advantage of the intermuscular coordination mechanism known as the crossover effect.21 The crossover effect occurs when the benefits from work done by one (uninjured) limb “crossover” to benefit the contraletal “uninjured” limb.
Most actions in team sports are related to the application of force in unstable situations. In fact, strength training on unstable surfaces (eg. squat on a bosu) has been shown to facilitate, among other things, greater co-activation of the quadriceps-hamstring muscles and greater activation of the core compared to the same exercises performed on a stable surface.22 In addition, stability training allows for high neuromuscular activation with little joint load or stress, which makes it very useful during the early phases of rehabilitation. However, unstable strength training does not allow athletes to achieve the levels of power or strength that can be achieved with stable strength training. Although there is no consensus on this, some research recommends combining training heavy loads under stable conditions with the aim of gaining greater power and strength with training lower loads under unstable conditions to obtain greater neuromuscular adaptations that promote joint stability (e.g. coactivation between quadriceps and hamstrings).22,23
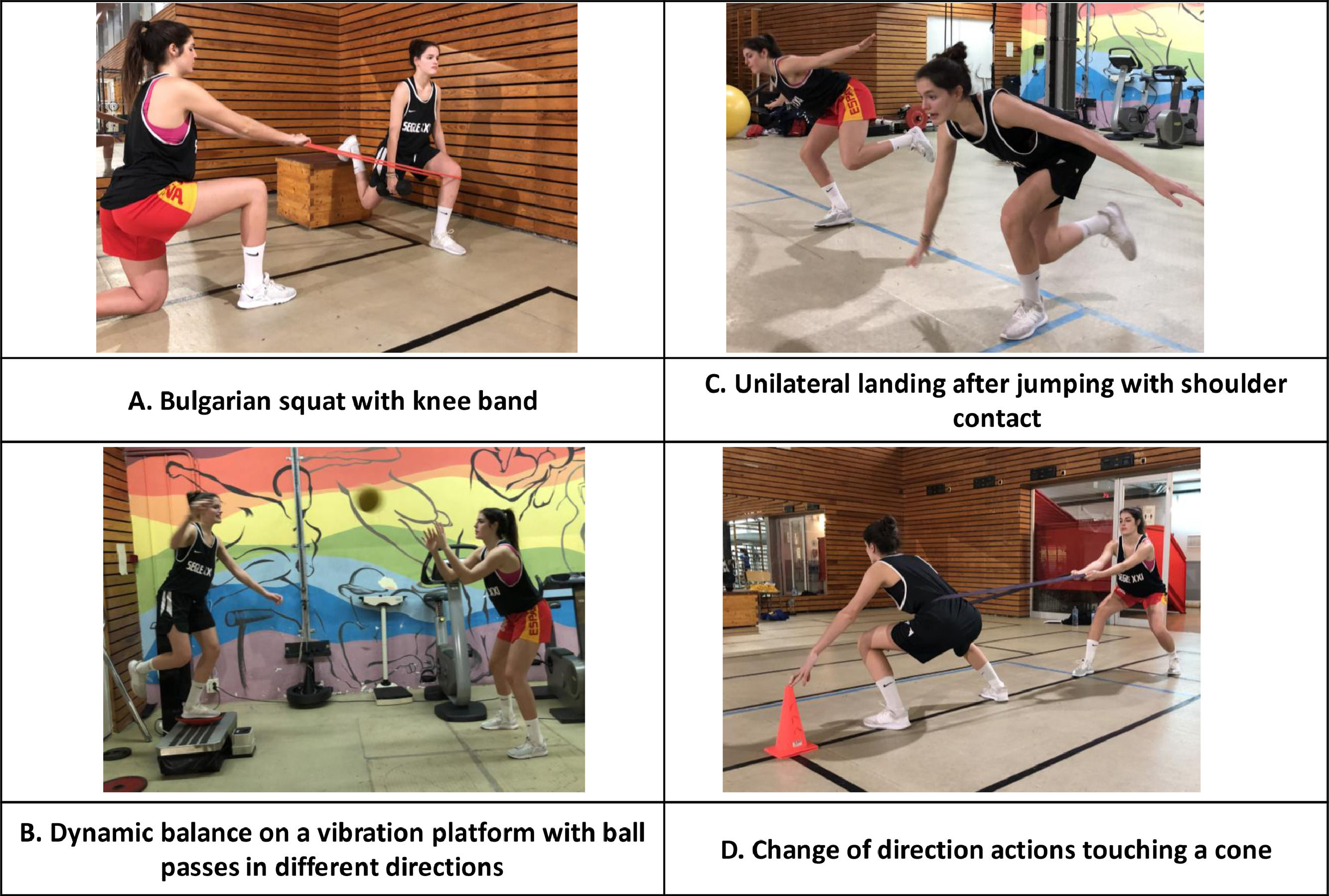
Compensatory workIn addition to prioritizing strength training of functional movements or the aforementioned fundamental movement patterns, it is also important to analytically approach muscles that have a more stabilizing function and that are associated with risk factors for ACL injury. This type of work is often called compensatory work (level of approximation 0-) and ecompasses tasks that reduce the risk of injury during functional movements (Figures 2 and 3). In the case of readaptation following ACL injury, the following muscles are especially important to knee stability, strength and precise muscle activation (neuromuscular control):24 (1) Quadriceps, in eccentric activation, (2) hamstrings, especially the medial part, (3) external rotators and hip abductors, (4) trunk, and (5) vastus medialis (related to the typical patellofemoral syndrome after knee surgery). In addition to the aforementioned muscles, decreased dorsiflexion25 can also be considered an area for compensatory work for ACL injury prevention since it promotes dynamic knee valgus, one of the main mechanisms of ACL injury.
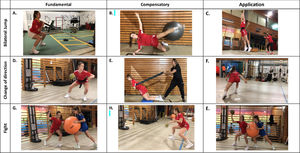
Example of strength and neuromuscular control tasks according approaching levels to RTC post-ACL injury in a volleyball player. The figure presents three level of approaching levels (0 - / 0+ / I) to improve strength and neuromuscular control in three areas: Lineal displacement, lateral displacement and bilateral jump. Level I examples are strength coordinative exercises performed through inertial equipment (A. Forward lunge with inertial device simulating forearm pass, B. Lateral step with forearm pass, C. Yo-yo squat reproducing a volleyball block), level 0+ examples are fundamental strength exercises with gravitational resistance (D. Unilateral hip trust, E. Lateral lunge with vibration, F. Hexagonal bar squat) and level 0- includes compensatory exercises (G. Single leg death lift with bosu, H. Running stork, E. Fitball kneeling with ball control).
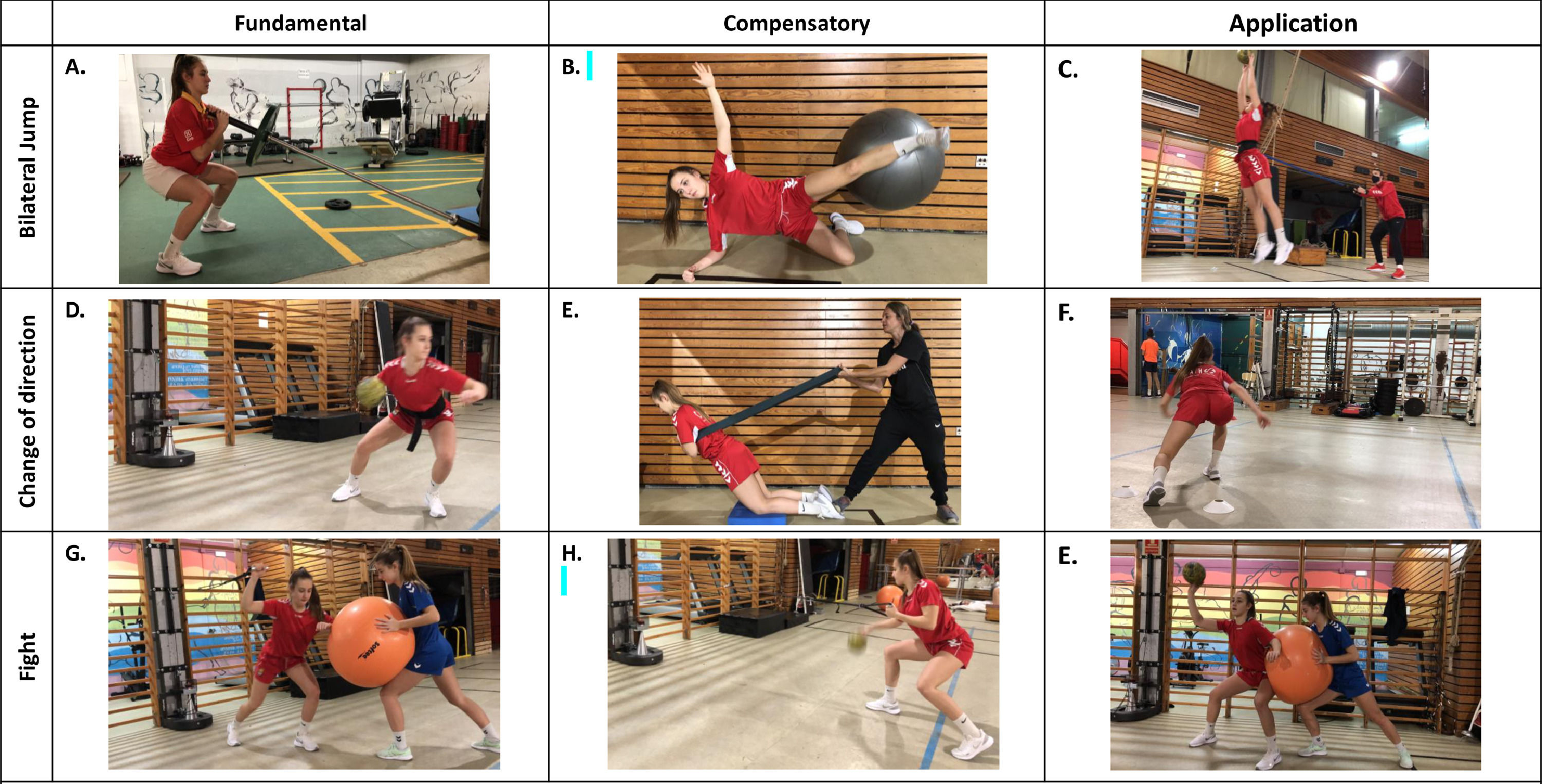
Example of the main part of a post-ACL RTC session organized in three chained exercises in a handball player. This session focus on coadjuvant training (emphasizing conditional and coordinative structure) and is organized by three training objectives (stations): 1 / Jump strength (A. Landmine squat, B. Core lateral clam, C. Jump simulating a defensive block); 2 / Change of direction strength (D. Crossover step with inertial device, pass and receive, E. Assisted Nordic hamstrings, and C. V-cut at maximal speed) and 3 / Fight strength (G. Unilateral pull press with partner perturbations, H. Unilateral row while bouncing, and C. Pivot position fighting and simulating a gain attack position.
Neuromuscular control depends on the sensorimotor system. It is described as precise neuromuscular activation that ensures dynamic joint stability and, in turn, enables coordinated and effective action.26 One of the main objectives during this phase is to achieve good neuromuscular control during the main fundamental motor skills (FMS) that compromise the injured structure. The main FMS following ACL-R in most team sports are running, jumping, and change of directions, which all involve the stretch-shortening cycle. These actions are associated with increased risk of ACL injury. Striking a balance between coactivation and reciprocal inhibition of the quadriceps and hamstrings is key to both protecting the knee and facilitating sport performance.27 To ensure proper mechanics (alignment and triple flexion of the hip-knee-ankle complex) during FMS (e.g. landings, change of direction), accurate neuromuscular activation of the hip abductors, trunk muscles and medial hamstrings are really important.28
Next, the bases on which to progress the difficutly of neuromuscular control tasks are described. Start with core work and lower limb dynamic stabilization and progress towards the retraining of the FMS, such as running, jumping (especially landings), and change of direction.
Dynamic core stabilityThe stability of the central part of the body (core), is essential to maintaining stability of the spine and proper lower limb mechanics (e.g. avoiding dynamic valgus in the jump landing) during sport actions.29
Our experiences and a review of the current literature suggest that dynamic core work should begin immediately following ACL-R with basic stability, mobility, and body awareness exercises. At this time it is very important to activate the deep muscles of the trunk (e.g. transverse abdominis and multifidus) and hip (e.g. gluteus medius) because low activation of these muscles combined with hyperactivity of the superficial muscles (e.g. rectus abdominis) is associated with injury, especially spinal injury.30,31
Once a good base of proprioceptive control of the core has been created, athtletes can progress towards more stable exercises to improve muscular endurance and capacity to react. It will then be possible to progress towards more specific exercises that load the core in the same what that training and competition do – during rotation, acceleration and deceleration actions.32
Lower limb dynamic stability: from balance to landingsThe current literature describes 3 categories of progression in dynamic stability training: a) static balance; b) dynamic balance and c) dynamic stabilization.33 Static balance is defined as the ability to maintain the center of mass on a fixed support base.34 This ability is highly influenced by the sensory information received, which is obtained through the somatosensory (especially proprioception), visual and vestibular systems.35 Once a good base of the proprioceptive-visual-vestibular system is created, athletes can progress towards improving dynamic balance. Dynamic balance is ability to maintain the center of mass on a fixed support base while experiencing disturbances, such as by balancing on an unstable base or by manipulating and/or controlling objects with other limbs.36 The disturbances effected in this second level of progression begin with controlled stimuli and progress towards unpredictable or unexpected situations.37 Finally, and as a guiding criterion to move on to RTS, the athlete should be able to tolerate dynamic stabilization tasks; that is, they should be able to maintain stability during/after dynamic actions, such as landing after a bilateral or unilateral jump in multiple directions with perturbations.38
When performing both the balance and dynamic stability tasks described above, it is recommended to focus on the correct alignment and triple flexion of the hip-knee-ankle complex (Figure 1). Previous research has shown how knee flexion during simple tasks, such as single leg balance (30°), or more demanding tasks, such as changes of direction, reduce valgus and increase coactivation between the quadriceps/hamstring muscles, both of which reduce the risk of ACL injury.6,39 In addition, it is also important to flex the trunk and maintain the physiological curvature of the trunk (lumbar lordosis), which will facilitate the activation of the hamstring muscles and further reduce the risk of ACL injury.
Training using vibration plates can also be useful in improving the dynamic stability of the injured complex.40 Coactivation of the quadriceps-hamstring muscles and the activation of the myotatic reflex (one of the main reflexes that works directly to facilitate balance and the stretch-shortening cycle) increase as a result of the vibratory stimulus. In addition, the vibratory stimulus produces a pain-inhibiting effect via the gate-control mechanism. This is very useful to improving neuromuscular control following damage to the cartilage, which occurs commonly following knee surgery.40 Several studies exist that demonstrate improvements to stability and neuromuscular control of the lower limb with vibration plate training following injury and during rehabilitation.41-43
Starting displacements: from running to change of directionThe main objective in this phase is to support proper mechanics of linear (front and back), lateral, diagonal and rotational movements. Table 3 shows a progression of tasks that aim to retrain the different movements based on approaching levels.
Task examples during retraining displacements after ACL-R in team sport following approaching levels.
First, it is important to achieve good symmetry in linear running. Some reserach suggests starting running around 12–18 weeks post-surgery, although this will depend greatly on the individual and especially if there are concomitant injuries.6,7,44 Training gait mechanics on soft surfaces (e.g. sand pit and/or graded treadmill) can be useful before starting running on solid ground.
Once an athlete has mastered a low speed straight run, they can progress towards a low speed lateral shuffle. The athlete can also progress to movements in multiple directions that include low impact changes of direction (e.g. 45°, 90° and 180°) at a controlled speed. It is important to train different angles of direction change to mimic sport movements and to train different types of maneuvers (e.g. side-step or cross-step). In Australian football, it was observed that ACL ruptures occurred during side-stepping maneuvers (37%), in landing (32%), land and step (16%), stopping/slowing (10%) and cross-over cut maneuvers (5%).45 Therefore, it is important to properly train these movements to mitigate ACL injury risk.
Useful tools to improve running and low impact multi-directional displacement include classic running technique exercises (e.g. skipping), coordinative exercises using ladders or something similar, and movements with resistance (e.g. incline treadmill or displacements with resistance bands).44
As the athlete tolerates the different movements, situations of deceleration (braking) and acceleration (starting) can be introduced at a controlled speed. Then, speed and complexity can be progressively increased.
Improve low impact resistance to fatigueIn most team sports, one of the keys to success is the ability to repeat high intensity bouts. This ability depends on capacity of the neuromuscular, metabolic and cardiorespiratory systems to adapt to fatigue. Fatigure-resistance plays an important role not only in performance, but also in injury prevention because neuromuscular fatigue is considered one of the biggest risk factors for sports injuries.46 Recently, high intensity interval training (HIIT) has become one of the most popular and effective methods for improving the cardiorespiratory, metabolic and neuromuscular systems.47 As long as the injured area allows, HIIT can begin in the initial stages of ACL rehabilitation. The conditioning program can progress from low-impact (eg. swimming, cycling, elliptical, etc.) to high-impact, such as running or change of direction drills.
Start SSS in a stable environmentDuring this phase, it is especially important to exclude the athlete from tasks that involve opposition and collaboration (1 vs 0), but to still include them in group training sometimes. For example, in basketball, injured athletes can participate in individual technique work with and without the ball, in a varierty of movements, like dribbling, changes of directions, changes of rhythm, reversals, etc. The athlete can also start making layups with changes of pace and direction. An important rule in this phase is that the technique must be prioritized over intensity. Once the technique is mastered (eg. good neuromuscular control during triple flexion of ankle-knee-hip), the athlete can progress towards an increase in the intensity of the action.
In order to progress to higher specificity levels, the injured athlete should be free of knee edema and have full range of motion (some degrees of knee flexion deficit may remain), good neuromuscular control of the FMS, and inter-limb strength asymmetry close to 70%3,7,8,48 When creating tasks closer to the competition, it is important to consider that the actions that determine the specific movements of team sports are changes of pace (accelerations and decelerations), the speed of movements, changes of direction, stride length and frequency; and all this adapting to the ball/implement, the teammates and / or opponents.49
Table 2 shows some useful tools and criteria to monitor and control the athlete's progression during the RTT period.7,31,50–52
Return-to-sportThis level of progression has the main objective of improving the injured athlete's sport-specific performance so that they can be reintegrated into training with the rest of the group.
At this time, sport-specific performance does not only consist of readaptation of the conditional and coordinative structures. It also consists of readaptation to skills at maximum intensity inside the variable and unpredictable environment (near chaos) typical of team sports, where emotional, cognitive and psychological structures play vital roles.
Furthermore, progressive increase of training load is key during this phase. At this time, it is very useful to have GPS/accelerometer devices and data to progressively increase the field load.53 In the absence of this technology, subjective questionnaires can be used that analyze the internal load (eg. Session-RPE or wellness questionnaires).54,55 While research is lacking, it seems to be useful to calculate the acute/chronic load ratios to avoid the typical “spikes”, or exponential increases, in load, which have been related to increased injury risk.56,57 Load becomes especially important when the injured athlete begins to rejoin group training sessions.
At the end of this phase, the athlete can begin to carry out full training sessions with the rest of the team. However, this does not mean that the athlete can perform all field workouts. At the outset, athletes can engage in, for example, two or three full field group training sessions, which is similar to the training load for most amateur teams.
Sport-directed strength developmentUntil now strength training has focused on hypertrophy and general coordination. When the structures are already prepared, the work of the coordinative strength can begin to be emphasized, that is, that strength directed to the sporting gesture and that the athlete must apply at each moment of the game (Approach level I → II → III). And, consequently, progress in specific and competitive strength training, that is coordinative work (technique of the sport itself) under the increase of external resistance.58
When following the structured training framework1 the main areas (basic skills) to reatrain post- injury are displacements (linear, lateral and rotational) and jumps (multiple directions, unilateral and bilateral) (Figure 2). These should begin in a controlled environment and progress towards a chaotic environment, which is specific to team sports. Improvements in strength and neuromuscular control during these actions will be key to enabling the athlete to tolerate sport-specific work.
As previously mentioned, team sports are characterized by wide variability in muscle activation patterns, which is why strength training aimed at sport movements must follow the path outlined here. Consequently, Moras (2017) proposes the construction of a variable training environment (3-dimensional and 4-dimensional) to compensate for the lack of specificity in classical strength training11, especially in the approach levels furthest from the competition (0-II). For example, in a change of direction exercise with a conical pulley can be varied by changing the distance, the bending angle, the number of steps, adding the ball, adding an unstable platform, or adding opposition, collaboration, shot actions or decision-making.
Most ACL injuries occur during the deceleration phase of jumping and/or direction changes59, which is why eccentric overload training takes an special relevance. From our experience, we observed that control of dynamic knee valgus during deceleration depends on the athlete's ability to both generate eccentric force in the extensors and activate the stabilizing muscles (e.g. hip abductors). Recently, several isoinertial devices that allow for eccentric overload during sport-specific tasks have become available18,60 (Figures 2 and 3).
To organize tasks in RTS sessions, it may be useful to use Seirul·lo's triseries (fundamental, compensatory and application exercises).1 This format is represented from the design of a fundamental exercise followed by a complementary or compensatory exercise and, finally, an application exercise. Fundamental exercises are polyarticular exercises that involve global movement and affect the main musculoskeletal system. Depending on the specificity of the session, the fundamental exercises will mimic the actions of the sport. The complementary exercises are characterized by recruitment of secondary muscle groups within the sport movement. Compensatory exercises help to minimize the risk of injury, and are aimed at correcting imbalances. Finally, the application exercises are those that facilitate muscular actions similar or identical to the technical gesture, reproducing both movement patterns and execution speeds. Depending on the levels of approximation of the exercises, actions that require decision-making can be included.61Figure 3 shows an example of the main part of a post-ACL RTS session that aims to improve strength and neuromuscular control (fight, change of direction and bilateral jump areas) organized in three chained exercises in a handball player.
Finally, it should be noted that in this phase training aimed at reducing neuromuscular asymmetries between legs during FMS and SSS is particularly important.62 Additionally, training should address asymmetries in both physical abilities (e.g. foot dorsiflexion, balance and/or strength) and motor skills (e.g. jumping and/or changes of direction in multiple directions). Research has shown that unilateral training is key to reducing inter-limb asymmetries resulting from injury.19,63 Once again, practitioners should monitor not only the magnitude of the asymmetry (with the Asymmetry Index), but also the direction of the asymmetry (eg. left vs right leg).62 Asymmetry becomes more important to address as the athlete approaches the end of the RTC process.
FMS at high intensity: unexpected actions and fatigue conditionsWhen retraining jumping and other movements in team sport athletes, it is important to keep in mind that using a knee-predominant strategy in the frontal plane has been associated with an increased risk of ACL injuries.64 In addition, the load on the ligament during changes of direction or landings increases with the decision-making, unexpected actions and fatigue65 typical of team sports.
In team sports, the intensity of actions depends not only on conditional and coordinative abilities (e.g. strength and power), but on perceptual and cognitive abilities. For this reason, good motor control strategies during FMS that involve the knee (displacements and jumps in multiple directions) in a closed and planned way must first be acquired. Then, open tasks, including decision-making, unexpected situations and fatigue conditions in game-specific situations, can be introduced progressively.66 In other words, the athlete must be prepared for the reality of the game, which includes adapting to the opposition, collaboration, fatigue and the pressure of competition. In this case, it can be very useful to have the so-called conditional-coordinative circuits. This kind of circuit training is widely used in the physical preparation of team sport athletes, and the nature and organization of the load resemble those of competition (Table 3). This type of work includes specific coordinative elements and nonspecific decision-making. From the conditional perspective, Circuit training allows for variations in work and rest times, which can place the emphasis on resistance to high intensity (longer duration with shorter rest) or on the speed of the action (shorter duration with longer rest). In addition, circuit training also allows sport-specific work on one or more specific motor skills through modification of the space and duration of the circuits. For example, to enhance high speed running in soccer players with circuits, we should introduce high intensity 20–30 m runs in a linear or near-linear path. Conversely, if what we want to enhance eccentric components of the actions, or increase the number of maximum accelerations and decelerations, we should introduce short and intense actions (e.g. stopping, changes of direction).
In order to prepare the injured athlete for unexpected game events, it is essential to train anticipation or pre-activation mechanisms (feedforward).26 Feedforward mechanisms have been associated with a greater ability to stabilize lower limb joints during risky situations, such as landings or changes of direction.67,68 In order to develop these protective mechanisms, it is important to introduce a wide variety of tasks and to gradually introduce unexpected actions.33
Finally, it is important to strike a balance between neuromuscular control (eg. correct technique and/or biomechanics) of the susceptible structures and the coordinative, perceptual and cognitive demands of the proposed task.
Improve resistance to fatigue in sport-specific environmentIn line with the previous section, in team sports one of the keys to success is the ability to repeat high-intensity bouts of effort.69 This ability is not only important for performance, but also plays an role in reducing the negative effects of fatigue (one of the major risk factors associated with ACL injury).66 In recent times, high-intensity interval training (HIIT) has become a popular method to improve respiratory, metabolic and neuromuscular capacity in team sport athletes.47 There are many potential applications for HIIT, including progressing from more basic skills in controlled situations to more specific skills in more unstable environments. For example, a possible progression of tasks from less to more demanding could be the following: 1) Classic HIIT with short intervals (eg. 15 s at high intensity - 30 s of active pause × 7 min × 2 sets), 2) repetitive sprint training with various changes of direction (eg 10 sets of 30 s - recovery 30 s) with minor decision-making, and 3) small games (eg. 5 sets of 3 min of half-court basketball).70 The possibilities for progressions are endless. It is important to consider integrity of the structure being retrained when progressing from a controlled environment to a chaotic, game-like environment.71
Combining SSS: progress towards a variable and unexpected environmentOnce the athlete is able to tolerate high-intensity SSS in a controlled environment, it is time to prepare the athlete for the reality of the sport: Fatigue + hyper-complex environment (unexpected situations where the athlete must make decisions based on their opponents, teammates, the ball/implement and decision-making with combined conditions). At this time, the athlete can begin to progressively train with the rest of the group. The athletes’ load should be closely controlled. When progressing tasks, it is important to consider the following aspects: 1) fatigue (e.g. training time), 2) number of high-risk motor actions (e.g. jumping and/or high intensity changes of direction), 3) decision-making (from simple to complex), 4) environmental disturbances (e.g. tasks with contact, and/or opponent, and/or the ball/implement), 5) collaboration (teammates), 6) and the degree of opposition. An example of task progression would be to start with situations without an opponent (1 vs 0, 2 vs 0…), progress towards situations of attach/defense (2 vs 1, 3 vs 2…), then reduced games (1 vs 1, 3 vs 3,… 5 vs 5), and end with real game (5 vs 5, 7 vs 7, 11 vs 11, etc. depending on the team sport).
Although there is currently no evidence on which factors succesfully predict RTC following ACL-R, it is recommended that practicioners use an extensive battery of tests in order to reach a consensus on RTC.3Table 2 shows some useful criteria and tools that can help determine how to progress from rehabilitation to competition.8,72,81,73–80
Return-to-competitionThe success of the rehabilitation is predicated on the athlete's ability to return at or above the preinjury level of competition without fear of reinjury influencing their performance. Key factors that determine readiness for RTC are the absence of pain and edema, preinjury or symmetrical strength and power in the lower limbs, ability to withstand repeated high-intensity bouts of effort, and good confidence and competence in technical and tactical performance (Table 2).82 In addition, readiness for RTC will depend on the athlete's level of play and on their psychological and social attributes.83 In fact, there is a scale that measures the athlete's psychological readiness to return to competition (ACL-Return to Sport after Injury scale).84
The decision to return to competion must be agreed upon by the different professionals that surround the athlete. Once a consensus is reached between the technical and medical staff, it is important to plan the progressive reintroduction to the team's competition, which will depend on the stage of the sport season. An example of how to progress in this phase would be to have an athlete start with low stakes competitive matches, such as exhibition games or competitions in lower levels of competition (eg. amateur). From here, the athlete will progressively increase the minutes of competition until they reach the highest level, which will match the demands of the competition. In this last phase, communication between the coach, player, and the rest of the staff takes on special relevance. It is important that the coach and the player talk about what is expected of one other and establish a plan to progressively return to competition at maximum performance while minimizing risk of reinjury.
It should be noted that the following aspects: being young, the absence of cartilage injuries, being a professional athlete, having a good psychological disposition, and good knee symmetry facilitate the success of RTC process.83
In order to faciliate competition at maximum performance, the athlete must continue to improve their ability to withstand different game scenarios, symmetrically refine their SSS (to the maximum extent possible) in real environments, and train with a competitive mindset to enhance security and confidence.
Return-to-peak performanceWhile an athlete may compete and even tolerate most of the training sessions with their teammates at pre-injury levels, this does not guaranteed that they have achieved their maximum potential. Team sports are characterized by weekly competitions where recovery time between games and training sessions is not always ideal. It is essential to monitor training and competition load because the neuromuscular and metabolic fatigue that characterizes team sports is one of the main risk factors for ACL reinjury.66 It is also important to progressively prepare the athlete to withstand the same loads as the rest of the team. As such, when returning athletes to competition they must be prepared to tolerate a match through exposure to progressive chronic load.56 Doing so will enable them to compete at maximum performance. It is crucial to avoid load spikes that typically occur when the athlete goes from a long recovery process to rejoining the normal competitive group. Technology (e.g. GPS, accelerometers and / or HR devices) is very helpful for this purpose.53
Specific preventionOnce an athlete has suffered an ACL injury, they must be educated about the importance of preventing reinjury. For these individuals, it is essential to evaluate ACL injury risk factors (Table 1. Part I) and to program in a way that reduces their risk of reinjury each season in a personalized way. Importantly, research shows that risk factors for reinjury (e.g. strength and dynamic stability asymmetries between lower limbs) can persist two years after returning to competition following ACL-R.85,86
Conclusions and practical applicationsRTS and RTC following ACL-R is challenging for team athletes. The RTS training program must be personalized, adapted to the training framework typical of team sports, and based on hypercomplexity. The planning of sports training takes on special relevance and the following key points stand out:
- -
Address and evaluate modifiable risk factors on an ongoing basis
- -
Progress in the specificity of the tasks
- -
Ensure good neuromuscular control in situations with high risk of ACL injury
- -
Introduce a wide variety of motor experiences
- -
Progress into an unpredictable environment full of disturbances/chaos
- -
Integrate perceptual and cognitive structures
- -
Prepare the athlete to perform under conditions of both fatigue and scoreboard pressure
Finally, we must highlight the importance of respecting two parts of the process: (1) the time needed for each player to progress, and (2) the coordinated effort that the professionals responsible for this process must make to ensure the athlete's individual optimal performance and RTC at maximal performance.
Laboratory(s) where the research was conducted: Catalan Council of Sport (Blume High Performance Center), Esplugues de LLobregat, Barcelona, Spain.