Proximal hamstring avulsions are a rare pathology, usually treated conservatively in elderly patients, resulting in severe functional limitation. Surgical repair can obtain a significant improvement in functionality and quality of life.
MethodsProspective case series of 3 women over 55 years of age (mean age 61), amateur athletes, with complete proximal and retracted hamstring conjoint tendon avulsion, treated by open primary repair surgery in chronic period (>4 weeks). The study variables were functional scales (PHAT, LEFS, and SF-12) before the intervention and one year after surgery, and strength measurement with a dynamometer and digital voltage scale. Statistical analysis included the Wilcoxon t-test and the Mann–Whitney U test.
ResultsOne year after surgery, all functional scales improved: PHAT 16 vs 83.33, LEFS 17.33 vs 68.67, P/SF-12.25.47 vs 51.14, and M/SF-12.35.42 vs 57.92. A normalization of the strength was obtained, observing a strength of 97.33% (range 72–140) and 111.67% (range 89–128) for contraction at 90° of flexion and in extension, respectively, with no differences between both legs. Digital measurement showed a strength of 99% (range 50–180).
ConclusionSurgery for complete and retracted proximal avulsions of the hamstring conjoint tendon in chronic period improves functionality and quality of life in elderly women with regular sports practice, as well as normalization of muscle strength.
The hamstring musculature is commonly injured during sporting activity. Most injuries occur as muscle strain or tears at the myotendinous junction.1 However, there is a more severe and less common form of injury2,3 that involves tendon avulsion at the ischial tuberosity.
Most proximal hamstring avulsions involve the conjoint tendon composed of the semitendinosus tendon (ST) and the long portion of the biceps femoris (BF). They usually occur during physical activity or after falls, as a result of hip hyperflexion with the knee in extension,4 with the age of highest incidence being between 45 and 59 years.5
The optimal treatment has not yet been clarified in the literature, although surgical treatment is recommended in most cases.6 However, most studies publish surgical results in middle-aged patients with regular sport practice,7 and not in older patients. This may suggest that in many cases, older patients tend to be under-diagnosed by downplaying the importance of the clinical findings8 or by lack of diagnostic means in consultation, and even in diagnosed cases, conservative treatment is chosen, based on the lower functional requirements of these patients. However, this can lead to severe functional limitation that compromises patients' quality of life, and to neurological side effects due to a hamstring syndrome.9
Outcomes after repair surgery are better in acute cases and partial injuries.7 In chronic cases, the worst results seem to be due to increased retraction and the appearance of adhesions,10 so early diagnosis may be essential for a correct clinical outcome.
The aim of the present study was to review the results after repair surgery in women over 55 years of age with complete, retracted and chronic proximal hamstring avulsion, after being treated conservatively in other centers and presenting significant functional limitation and secondary neurological symptomatology. To date and to the knowledge of the authors of this study, there is no cohort with these characteristics published in the literature.
Material and methodsWe present a prospective case series consisting of a sample of 3 women over 55 years of age (mean age 61 years) treated surgically in our center for proximal hamstring avulsion between the months of March and September 2021, after being rejected for surgery in other centers.
Inclusion criteriaInclusion criteria were complete avulsion with retraction of the proximal hamstring conjoint tendon, a surgical delay of at least 4 weeks since the initial injury, an age equal to or greater than 55 years, and a regular practice of sports at an amateur level. Partial injuries, acute repairs, patients younger than 55 years of age, and patients who practiced sports at high level were excluded from the study.
Clinical and epidemiological dataIn all cases, epidemiological data, mechanism of injury and previous level of physical activity were collected. Personal history, physical examination, the Perth Hamstring Assessment Tool (PHAT), Lower Extremity Functional Scale (LEFS), 12-item Short Form Survey (SF-12), and complementary exams were collected, including ultrasound in consultation and confirmatory Magnetic Resonance Imaging (MRI) (Fig. 1). The surgical delay was also recorded, counted in weeks (Table 1).
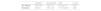
Clinical and epidemiological data and surgical delay.
Values in absolute cases and percentages in parentheses (categorical variables) or in means and standard deviations (continuous variables).
The surgical procedure consisted in an open reduction and anatomical fixation of the tendons in the ischial tuberosity. To this purpose, the level of retraction of the stump was first referenced by ultrasound for the surgical incision, which was longitudinal and centered on the conjoint tendon (Fig. 2a and b). After the approach, the sciatic nerve was located first. After neurostimulator-guided neurolysis of the nerve, the tendon and musculature were exhaustively released to achieve its complete mobilization, allowing an anatomical reduction. Finally, after debridement of the insertional footprint in the tuberosity, fixation was performed with 3 or 4 anchors (double or triple) using the Krakow technique with a sliding and self-locking knot to achieve the reduction and mattress configuration to provide compression to the repair (Figs. 3 and 4). Subsequently, platelet-rich plasma (PRP) was infiltrated intratendinously, peritendinously, intramuscularly and perineurally. Thanks to complete myotendinous mobilization, it was not necessary to use graft in any case, regardless of the level of retraction.
Postoperative rehabilitation was divided into 3 distinct phases:
- 1.
During the initial phase (4–6 weeks period) partial weight bearing was performed with the aid of crutches, walking with the affected limb in extension and external rotation in order to activate the adductor musculature, thus avoiding hamstring contraction and immobilizing orthoses for active knee flexion restriction. Physiotherapy in this phase was based on passive assisted mobility exercises of the foot and hip in all planes, avoiding hip hyperflexion, as well as introducing isometric exercises of the unaffected musculature.
- 2.
During the middle phase (6–12 weeks period) active mobility was started, progressively removing the crutches and returning to normal gait. In this phase, the static bicycle without resistance and controlled stretching were introduced.
- 3.
During the final phase (from the 3rd month onwards), strength-gaining exercises were started with low-impact activities as long as the patient did not present pain, with increasing intensity as tolerated. Physiotherapy was focused on improving range of motion and motor control, as well as introducing eccentric loading and proprioceptive exercises.
Follow-up had a minimum duration of one year, at which point the PHAT, LEFS and SF-12 tests were repeated. Strength assessment was also performed with a manual test using a dynamometer in prone position, performing contraction at 90° of knee flexion and contraction in full extension, measured in kilograms (Fig. 5a and b). In addition, an explosive strength test was performed using a digital power scale (Enraf-Nonius - ©), measured in Watts, consisting of 2 series of 8 reps with progressive weight load (Fig. 6a and b).
Statistical analysisFor statistical analysis, the nonparametric Wilcoxon t-tests for related samples and Mann–Whitney U-tests for related samples were performed using the SPSS program (IBM). A value p <0.05 was established as statistically significant.
ResultsThe mean time from injury to surgery was 12.67 weeks (SD 11.55). The mean myotendinous retraction was 6.33 cm (SD 1.53) measured by ultrasound, and 7.5 cm (SD 4.92) measured by MRI.
Functional tests were performed prior to surgery and repeated at one year postoperatively, all of them showing significant improvement. The PHAT scale increased from a mean score of 16 to 83.33 (p = 0.109), while the LEFS increased from a mean score of 17.33 to 68.67 (p = 0.102), the physical component of SF-12 (P/SF-12) from 25.47 to 51.14 (p = 0.109), and the mental component of SF-12 (M/SF-12) from 35.42 to 57.92 (p = 0.109) (Table 2).
Functional scales performed before the intervention and 12 months after surgery.
| BS | 12 months | p-value | |
|---|---|---|---|
| PHAT (0-100) | 16±3.61 | 83.33±7.64 | 0.109 |
| LEFS (0-80) | 17.33±3.79 | 68.67±4.16 | 0.102 |
| P/SF-12 | 25.47±6.06 | 51.14±6.69 | 0.109 |
| M/SF-12 | 35.42±3.55 | 57.92±0.93 | 0.109 |
Values presented as mean ± standard deviation. PHAT (Perth Hamstring Assessment Tool); LEFS (Lower Extremity Functional Scale); P/SF-12 and M/SF-12 (physical and mental components of the 12-item Short-Form Health Survey, respectively); BS (before surgery).
The strength assessment obtained similar results when comparing the operated leg with the non-operated leg. The manual dynamometer test showed for the contraction at 90° of flexion a 97.33% of strength with respect to the contralateral (one of the cases presented 140%, p = 0.637). For the contraction in extension, the test showed 111.67% vs. the contralateral (in this case two patients presented 128% and 118%, p = 0.827) (Table 3).
Manual dynamometer test. Contraction measurement at 90° of flexion and in full extension.
| Operated | Not operated | %diff. | p-value | |
|---|---|---|---|---|
| 90° Flexion | 5.33±1.53 | 5.67±1.15 | 97.33±37.17 | 0.637 |
| Extension | 6.5±2.5 | 5.67±1.26 | 111.67±20.26 | 0.827 |
Values presented as mean ± standard deviation, units of measure in Kgs. % diff. (% difference of the operated leg with respect to the non-operated leg).
In the explosive strength test with digital scale, when compared with the contralateral leg, a mean of 99% of strength measured in Watts was obtained (range 50–180%, p = 0.513) (Table 4).
DiscussionThe most relevant finding of the present study is that surgical repair of complete proximal hamstring avulsions has good outcomes in athletic patients of advanced age and chronically injured, allowing them to recover their quality of life.
The type of treatment has been subject of debate in the literature, but there has been a clear tendency in recent years towards surgical treatment, as it obtains better results in complete avulsions. The most widely used classification for proximal hamstring avulsions is the one established by Wood et al.11 based on MRI findings, and is the one mostly used to establish the surgical indication. Surgery is generally indicated in the active population with an avulsion of 2 or more tendons with 2 cm or greater retraction (Wood type 5), or after failure of conservative treatment for 3–6 months in the remaining cases.12,13,14
Systematic reviews have been published in the literature recently with satisfactory results after surgical treatment of this pathology. These studies focus the surgeries on middle-aged patients who practice sports activities regularly. Hillier-Smith et al.,7 in their review of 1530 patients treated surgically, present a mean age of 44.7 years, which is similar to other systematic reviews with ages of 39.713 and 41.4.6 However, in our case we are dealing with older patients (mean age 61 years) with less sporting activity, who are usually underdiagnosed or ruled out for surgery for these reasons. All of them had disabling functional symptomatology, so conservative treatment was not a viable option in these patients.
The time to surgery has also been studied recently. In the present work, the results are very favorable despite the chronicity of the lesions, something that shows disparity in the literature. Most studies conclude that acute surgery obtains better results than chronic injury treatment in terms of function,8 satisfaction, return to sport and strength test.15–19 In contrast, in their systematic review van der Made et al.9 report minimal or no differences between acute or chronic treatment, although the main relevance lies in the poor quality of the included studies. Coughlin et al.20 conclude in their review that there are no differences between acute and chronic treatment in terms of sporting return, arguing that the definition of chronicity varies between studies, which may influence the results.
There are several possible reasons for the inferior results in chronic cases. From a technical point of view, acute repairs tend to be less demanding than chronic cases as they involve less scar tissue in the area of injury and the anatomy is more easily defined. In addition, in chronic cases a large amount of stump retraction can be found, which can compromise the intervention and be one of the factors that lead to a better outcome in acute repair. These worse functional results obtained in chronic injuries10 may also be due to progressive and irreversible muscle atrophy and fatty infiltration caused by non-repair of the tendon. In addition, chronic repairs can result in a thickened tendon, which if not sufficiently prepared can lead to pain over the tuberosity with sitting, impaired physical activity, etc., a factor that was not present in the patients of this study, possibly due to an anatomical fixation in the footprint, which has a proximal and lateral location within the tuberosity. On the other hand, the amount of stump retraction has not been associated with a worse functional outcome,10 which may indicate that it is the amount of fibrosis and adhesion of the stump that makes the repair more challenging, which in turn is conditioned by the surgical delay in chronic cases. For these reasons, and based on the results of this study, it is confirmed that a surgical technique that includes a exhaustive tendon and muscle release and preparation can lead to good clinical and functional results in chronic cases. There are other published studies that treat complete avulsions in the chronic period using graft delivery as a salvage technique,21,22 which may be another factor influencing the inferior results presented.
According to recent literature, only 2 tools have been validated specifically for hamstring repair, the Perth Hamstring Assessment Tool (PHAT)23 and the Sydney Hamstring Origin Rupture Evaluation (SHORE). Of these, the PHAT is the most widely used, although curiously in a recent systematic review it was only included in 16.7% of the studies reviewed,16 which may indicate an inaccurate functional outcome assessment in many of the publications. In another recent systematic review,24 after analyzing the different outcome measures of proximal hamstring injuries, it is concluded that the PHAT is the most specific tool, although the LEFS can show improvements in sports activity in athletes, and the SF-12 provides a perspective of the mental component that would result in a more complete outcome analysis.
In the current study, the results of the functional tests used (PHAT, LEFS, SF-12) indicate a substantial improvement in clinical function after surgical treatment regardless of the chronicity of the injury, improving the quality of life of the patients. Interestingly, there is not only an improvement in the physical tests, but also a substantial improvement in the mental component of the SF-12, which indicates that these lesions condition an affectation of the psychosocial status that is important to take into account when determining the treatment. These results are slightly higher than those obtained in other studies dealing with complete and chronic avulsions, such as by Ebert et al.21 who report a mean PHAT of 67, a mean LEFS of 63, a mean P/SF-12 of 46 and a mean M/SF-12 of 51.9 one year after surgery with a technique involving ipsilateral distal ST graft supply. In turn, the article by Factor et al.25 obtained a mean PHAT of 73 with an endoscopic and mini-open technique. In the longest systematic review to date,7 a mean LEFS of 74.7 is reported, with differences between partial and complete lesions (76.4 vs 73.3), but not between acute and chronic repairs (74.5 vs. 74.7).
Regarding postoperative strength, dynamometric measurements and voltage tests show a strength around 97% with respect to the healthy leg, which represents a normalization of the latter after surgery. These results are slightly higher than those of other published studies, despite treating younger patients or acute repairs (85%6), and comparable to the normalization obtained in other studies of complete chronic injuries.25 In the present study, the greater strength obtained in some of the patients may be conditioned by specific rehabilitation of the operated leg and less training of the healthy leg compared to patients with a high level of sports activity. Hillier et al.7 found no significant differences between acute and chronic repairs (89.8% vs. 90.8%) but did find significant differences between partial and complete injuries (90.5% vs. 84.4%, p = 0.000). These results seem to indicate that complete injuries present a lower strength recovery and greater functional limitation due to the severity of the injury itself, although the results in chronic repairs may be comparable to acute repairs, which is in line with the results of this study.
The main limitation of this study is that it consists of a small sample size. However, this is a very specific cohort of elderly patients who are usually ruled out for surgery, so this sample may be of great clinical interest and the results may help in making therapeutic decisions for this type of lesion among these patients.
To date, to the authors' knowledge, no articles have been published with a sample of these characteristics, but for greater certainty, it is necessary to increase the series and to carry out prospective and randomized studies in the future.
ConclusionSurgery for complete and retracted proximal avulsions of the hamstring conjoint tendon in chronic period improves functionality and quality of life in elderly women with regular sports practice, as well as normalization of muscle strength.