Introducción: La ecografía convencional permite identificar los cambios macroscópicos que se producen en el tendón patológico; sin embargo, estos cambios no se correlacionan bien con los síntomas o la respuesta al tratamiento. La Ultrasound Tissue Characterization (UTC) evalúa la estructura del tendón en 3 dimensiones y la clasifica en 4 ecotipos. El objetivo de este estudio fue investigar la estructura del tendón rotuliano de jugadores de baloncesto utilizando la técnica de la UTC y estudiar las diferencias entre jugadores profesionales y formativos, comparando la pierna dominante con la pierna no dominante, y sintomáticos con asintomáticos.
Material y métodos: Un total de 40 tendones rotulianos (20 jugadores de baloncesto) se incluyeron en el estudio. La estructura del tendón rotuliano (proximal, medial y distal) se cuantificó mediante UTC en el inicio de la pretemporada. La fiabilidad inter e intraobservador se estudió mediante el coeficiente de correlación intraclase (CCI).
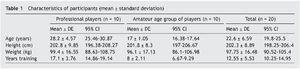
Resultados: La edad media de los 10 jugadores profesionales y la de los 10 jugadores formativos fue de 28,1 (DE 4,5) y 17,6 (DE 1,13) años, respectivamente. El espesor del tendón rotuliano fue mayor en los jugadores profesionales (p < 0,05), en la pierna dominante (p < 0,05) y en los tendones sintomáticos (p < 0,05). No se encontraron diferencias significativas para los ecotipos, excepto en el caso del ecotipo ii del tendón rotuliano derecho en la porción proximal entre los jugadores profesionales y los académicos (p = 0,05), y en los ecotipo iii y iv del tendón derecho en su porción proximal entre los jugadores sintomáticos y los asintomáticos (p < 0,05). Se encontró una buena-alta fiabilidad con estas técnicas (CCI = 0,80-0,99).
Conclusiones: Se ha caracterizado el patrón ecográfico de los tendones rotulianos de jugadores de baloncesto utilizando UTC. El espesor del tendón rotuliano es mayor en los jugadores profesionales que en los jugadores académicos. También se ha observado mayor grosor de los tendones sintomáticos que de los asintomáticos. No hubo diferencias importantes en el patrón de UTC entre los jugadores profesionales y los académicos ni entre los sintomáticos y los asintomáticos.
Introduction: Conventional ultrasound assists in identifying the macroscopic changes produced in the injured tendon. However, these changes do not correlate well with the symptoms or the response to treatment. The ‘characterisation of tissues by ultrasound’ (UTC) evaluates the structure of the tendon in 3 dimensions and classifies it into four echo types. The aim of this study was to investigate the structure of the patellar tendon in basketball players using the UTC technique, and to study the differences between professional and amateur players by comparing the dominant leg with the non-dominant one, and symptomatic cases with asymptomatic ones.
Material and methods: The study included 40 patellar tendons (20 basketball players). The structure of the patellar tendon (proximal, medial and distal) was quantified by UTC at the beginning of the pre-season. Within and between observer reliability were measured by intraclass correlation coefficient (ICC).
Results: The mean age of the 10 professional and 10 amateur players was 28.1 years (SD 4.5) and 17.6 years (SD 1.3), respectively. The thickness of the patellar tendon was greater in the professional players (P < .05), in the dominant leg (P < .05), and in symptomatic tendons (P < .05). There were no significant differences in echo types between professional and amateur players (P = .05), except in the case of echo type 2 in the proximal portion of the right patellar tendon. Similarly, there was a difference in echo type 3 and 4 of the proximal portion of the right tendon between symptomatic and asymptomatic players (P < .05). Good, high reliability was found with these techniques (ICC = .80-.99).
Conclusions: The ultrasound pattern of patellar tendons in basketball players was characterised using UTC. This tendon was seen to be thicker in professional players than in amateur players. It was also observed that symptomatic tendons were thicker than asymptomatic tendons. There were no significant differences in the UTC patterns between professional and amateur players, or between symptomatic and asymptomatic players.
Introduction
The tendon is a mechanically sensitive connective tissue that responds to short (24-72 h) and long-term (12 weeks-years) load changes.1 Patellar tendinopathy is a very common pathology in athletes, with a prevalence of 55% in basketball players,2 associated with overload from many years of sport.3
In the case of Achilles tendinopathy, disintegration of the collagen matrix can be seen as a consequence of degeneration, forming fibrotic tissue in response to the repair.4 With conventional ultrasound, tendon echogenicity is based on the density and arrangement of the collagen matrix, producing a grayscale pattern, however, this is insufficient to be able to monitor and objectify changes in the internal echo-structure over time.5,6 At the other extreme, the disintegration of the fascicles leads to a considerable loss of echogenicity. Consequently, hypoechoic lesions are frequently described in cases of tendinosis,7 in addition to observing other findings, such as tendon thickening and increased echo-Doppler signal.8,9 However, there is no clear correlation between these changes and the symptomatology,10 or in improvement, after applying different treatments.11 Recently, a new imaging technique: ultrasound tissue characterisation (UTC), has been developed. Through the use of ultrasound in mode B, this technique evaluates the three-dimensional structure and quantification of tendon organisation by analysing the stability of pixel brightness, making it possible to classify this into 4 echo types, which correlate with the degree of homogeneity (fibrillary alignment) of the tendon.5,6
Most UTC studies have examined the Achilles tendon in racehorses12 and in Australian football players,13 and there are few which analyse the patellar tendon. Of the studies that analyse this tendon, it has been observed in volleyball players that the tendon structure is not affected over the course of 5 days of accumulated load during a tournament.14 However, more studies are needed to analyse how the patellar tendon is affected in other sports, such as basketball.
We embarked on this study due to the lack of studies that analyse the changes that occur in the process of adaptation and injury of the patellar tendon in competition basketball players. The objective was to analyse the pattern structure of the patellar tendon by characterising 4 different echo types using UTC, in addition to defining a pattern for normal tendons in basketball players and looking for differences between professional players and amateur players, in addition to differences between symptomatic and asymptomatic cases.
Material and methods
Participants
In August 2015, a total of 40 right and left patellar tendons were analysed in male basketball players, with 20 professional players (n = 10) and 20 players in amateur ages ranges (n = 10). The inclusion criteria were as follows: (i) aged between 15 and 35 years old, and (ii) being members of the same club. Exclusion criteria were considered to be: unsystematic tendon treatment over the last 6 months, treated with substances such as glucocorticoids, fluoroquinolones or hormone replacement therapy, nor having suffered hypercholesterolemia or any rupture in the patellar tendon.
This study was approved by the local Ethics Committee and all participants signed an informed consent form prior to starting the study.
Clinical assessment
All players were assessed clinically and jointly by the first team (GR) and second team (GH) physicians. Height, weight, age, years of basketball practice and the presence or absence of symptoms of patellar tendinopathy over the previous two seasons were recorded. Of the 20 players, 12 had had symptoms in the dominant knee tendon, on at least two occasions each season, over the previous two years. At the time of the test all players were asymptomatic for patellar tendon pain. Table 1 shows the characteristics of the sample analysed.
Assessment by ultrasound tissue characterization
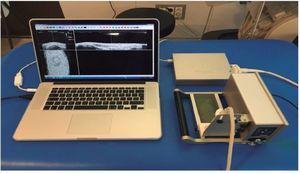
All assessments were made during the early morning in pre-season: players in the amateur age range on 18 August, and professional players on 25 August. The same expert in ultra-sonography and UTC (GH) examined both patellar tendons by ultrasound in mode B with a linear transducer of 7-10 MHz (SmartProbe 10L5; Terason 2000, Teratech, USA), mounted on a device that moves the transducer automatically along the perpendicular axis of the tendon, and which records cross-sectional images at intervals of 0.2 mm over a distance of 12 cm (600 axial images) (Figure 1). The device standardised the probe’s angle of inclination, the gain, focus and depth. Images were captured and UTC measurements taken following a standardised protocol applied in other studies.6
Figure 1 Apparatus used for measurements. UTC device.
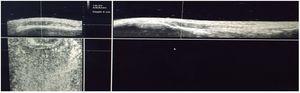
The player positioned himself with his knee bent at 90° and his foot resting on a raised surface. The device was placed parallel to the long axis of the patellar tendon, from its distal insertion in the anterior tibial tuberosity to its proximal insertion at the lower end of the patella. Gel was applied between the skin, the silicone support, and between the silicone support and the ultrasound probe, before running the scan (Figure 2).
Figure 2 Positioning of patient and UTC system.
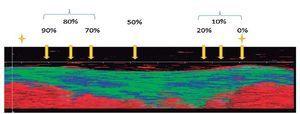
Seven areas of interest were calculated from the total free length of the tendon: proximal (0, 10 and 20%), medial (50%) and distal (70, 80 and 90%) (Figure 3). The proximal, medial and distal anteroposterior (AP) diameter was calculated as the free length of the patellar tendon, from the proximal insertion at the lower end of the patella to the most prominent part of the anterior tibial tuberosity at the distal end (Figure 4).
Figure 3 Distribution of patellar tendon areas of influence.
Figure 4 Initial assessment of patellar tendon and measurement area.
The echo pattern of the UTC was quantified by one same blind observer for the patient's history. For each proposed cut-off point, the region of interest (ROI) was determined. The observer identified the ROI by drawing it around the edge of the tendon in the cross-sectional view. The echo pattern was analysed by the UTC software itself (UTC 2010), used for the scan at each cut-off point. The software inserts the ROI by creating tendon volume where the proportion of each echo type (1, 2, 3, and 4), based on the stability of the pixel brightness across continuous images, enables correct alignment of the fibres to be assessed (Figure 5).
Figure 5 Distribution of tendinous patellar fibres by region and echo type.
The 4 validated echo types can be discriminated between and related to tendon integrity. Echo type 1 represents the intact, continuous and aligned fascicles. Echo type 2 represents the less continuous and/or more undulating fascicles. Echo type 3 represents a mainly fibrillar matrix. Echo type 4 represents complete disintegration with liquid-substituted connective tissue and an amorphous matrix.5,6
Interobserver and intraobserver procedure
The analysis procedure was run by two independent observer physicians (GH and DD) who evaluated 10 different tendons at 3 different points in time, between 5 and 15 days. Both observers had the same length of experience using UTC.
Statistical analysis
In order to analyse intraobserver and interobserver variability in 10 patellar tendons at the proximal, medial and distal levels for all echo types, the intraclass correlation coefficient (ICC) was used applying the following criteria: 0.9-0.99, high reliability; 0.8-0.89, good reliability; 0.7-0.79, normal reliability; < .69, poor reliability.15 ICC was used to assess the correlation between one researcher’s observations and those of different observers. All statistical analyses were run with the use of the IBM SPSS Statistics package (v.21), with an assumed significance of P < .05.
Results
Reliability of intra-observer and inter-observer UTC
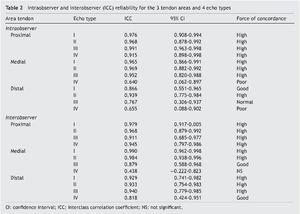
Table 2 shows the results obtained for the two different levels of analysis (intraobserver and interobserver) for the three zones of the tendon and the four different echo types. For the intraobserver level, the results showed high reliability for all four echo types in the proximal tendon area (P = .001). For the medial area, high validity in echo types 1, 2 and 3 was also seen, with echo type 4 reflecting lower reliability (P = .017). For the distal area, echo types 1 and 2 showed high or good reliability (P < .001), while for echo types 3 and 4 this was low or poor (P = .014). For the inter-observer level, the proximal zone also presented high reliability for all four echo types (P = .001). The medial and distal areas showed high reliability for echo types 1 and 2 (P < .001). For echo type 2, reliability was good in the medial area, and high at the distal end (P < 0,001). In terms of echo type 4, there was high reliability in the proximal area (P = .001), good reliability in the distal area (P = .001) and poor (non-significant) reliability in the medial area.
The study of inter- and intraobserver variability by ICC in the proximal, medial and distal areas for all echo types showed very high reliability and repeatability of the technique between 0.90-0.99 (P < .001 ), following the criteria of Currier, 1990.15 This enabled us to run the analyses with different observers without altering the result.
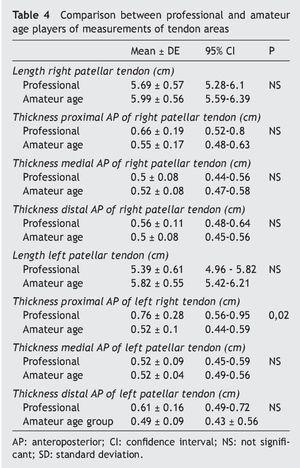
Comparison of tendons between professional players and players in the amateur age range
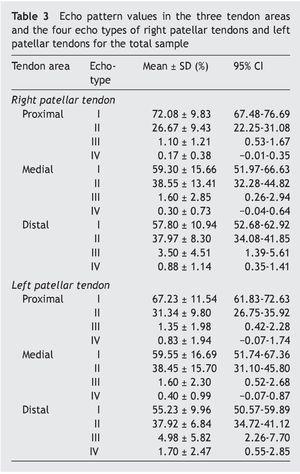
Table 3 shows the descriptive values of the echo patterns in the 3 different areas of the tendon (proximal, medial, and distal) and the four echo types for the total of the sample. Table 4 shows the results obtained from the comparison between the two groups of players for the measurements of different areas of the tendon. The results only show significant differences in the proximal AP thickness of the left right tendon between professional players and players in the amateur age range (P = .02), as well as in symptomatic tendons (P < .05). For the rest of the tendon areas no significant differences were observed between the two groups of players.
Discussion
Due to the lack of studies that have analysed the changes taking place in the process of adaptation and injury of the patellar tendon in competitive basketball players, we began this study with the objective of analysing the pattern structure of the patellar tendon, characterising 4 different echo types using UTC. In addition, the study aimed to define a pattern of normal tendons of basketball players and seek differences between professional players and players in the amateur age range, in addition to differences between symptomatic and asymptomatic cases.
If we focus on the values for tendon thickness in the 3 areas measured, it can be seen that the patellar tendons are thicker in professional basketball players, and in players who present clinical symptoms (whether or not professionals). Likewise, it was shown that there are no significant differences in the pattern of UTC echo types between professionals and amateurs, or between players who do not present symptoms and those who do.
The fact that there are no significant differences in the relative percentages of echo types, despite years of training and the presence of symptoms, indicates that the intrinsic structure of the tendon is maintained, i.e. there is no failure in repair, as one model has proposed16, but probably a process of adaptation of the tendon to the workloads. These results are in line with the model, proposals17 and recent findings by Docking and Cook (2016)18, who argue that there is an increase in echo type 1 after 5 months of training. This would also explain the improvement of echo types in the UTC image after loading periods, and the greater presence of echo type 1 in sportsmen, along the same lines as observed in this study. What seems clear is that the increase in tendon thickness is an adaptive response, since the increase in thickness reduces the stress on the tendon structure (force/CSA).19
It is striking that there was a tendency towards a slight increase in echo type 1 in the right-hand tendon (non-dominant leg) in comparison with the left (dominant leg) and the tendency towards more echo type 2 in the left patellar tendon (dominant leg) than in the right (non-dominant leg). These tendencies in the patterns were observed in the proximal, medial and distal tendons. These findings concur with the different biomechanics of each leg in basketball and the different loads to which they are subjected during the practice of this sport.20
Unlike Wezenbeek et al.,21 the main echo types are always type 1 at both insertion point and medial portion — although it is true that the study by Wezenbeek et al. was performed on Achilles tendons. In the same study by Wezenbeek et al. there are differences between the insertion region (greater amount of echo type 2) and the medial region (majority of echo type 1). This is not the case in the present study, where echo type 1 predominates in all tendon regions. Although healthy subjects were studied in both studies, the differences are probably due to differences between the patellar and the Achilles tendon.
The high percentage of echo type 2 regions is remarkable, even though the assessment has been done in healthy subjects. These findings may be surprising but if compared with other recent studies13,14,18 it can be seen that coexistence in the same tendon of these two echo types is common. Rosengarten et al. contended that the combination of both echo types in the same tendon was due to the fact that the normal integrity of the tendon was being negatively affected by either excess load or other risk factors.
Patellar tendinopathy is a very common pathology in basketball, both professional and amateur, but only exceptionally does this lead to a break in training, since with suitable local rehabilitation, specific rehabilitation work and the strict control of loading, this is a pathology that is relatively well-tolerated and enables sport to be continued with no excessive difficulty. This rehabilitation treatment and directed and controlled monitoring of load-bearing is likely to aid the adaptive process of the tendon, thus favouring the disappearance of the clinical symptoms. In this adaptive process in the tendon, changes can be observed in the tendon structure in the imaging tests, without necessarily presenting any clinical symptomatology.20,22
The results obtained reveal the need to continue research into the analysis by UTC of tendons in athletes competing in the different sports disciplines. This would enable us to establish patterns of normality according to different athletes, their load intensity and the sport discipline that they practice, in addition to being able to compare these results with those of other sports.
Conclusion
The pattern of echo types in the patellar tendon, as yet not described in basketball has now been characterised by UTC. The patellar tendon is thicker in professional and symptomatic athletes, probably because of an adaptive effect. There were no significant differences between professionals and amateurs as regards the pattern of UTC echo types, or between symptomatic and asymptomatic cases. In this study it was also shown that the UTC technique reveals good intra- and interobserver repetition for use by experts.
Prospects
In the future we believe that we should study the effect of the impact of maximum load over a prolonged period — for example over a whole season — on the tendon structure and observe the changes that occur (this team, in particular, undergoes an average of 290 training sessions per year and plays more than 80 matches).
In addition, it will also be important to analyse and monitor symptomatic tendons throughout the season to ascertain whether UTC enables us to evaluate changes in the echo structure when a reduction in load is prescribed or biological treatment is given.
Conflict of interest
The authors declare no conflict of interest.
Received 12 October 2016;
accepted 11 November 2016
☆ This paper forms part of a research project for the doctoral thesis of Gemma Hernández, Universitat Autònoma de Barcelona, Department of Surgery.
* Corresponding author.
E-mail address:drpedret@gmail.com (C. Pedret).