The long recovery time required after deep venous thrombosis (DVT), or other serious manifestations of venous thromboembolic disease, can lead to a reduction in sporting condition and economic losses. Neither are such events always free of clinical sequelae.
ObjectiveThis study examines the prevalence of DVT in male, professional soccer players in Spain.
MethodsA questionnaire on DVT events experienced by players in the ongoing 2015-16 season, and the previous 10 seasons, was sent to the medical services of all first and second division clubs in Spain. The genetic predisposition of those who suffered an event was investigated using the inCode thrombus test, as well as in 73 players who experienced no such event.
ResultsFour subjects were diagnosed with DVT via clinical history and ultrasound or D-dimer determination. This associated prevalence (1.2/1000) is higher than reported (1/10,000) for this age group in the general population (18-35 years). All four affected players carried a risk allele (A1) at the ABO locus, three were homozygous for the risk allele of FactorXIII, and one was heterozygous for a risk allele of FactorXII. Among the 73 players who experienced no DVT, 3 high risk genetic variants associated with thromboembolic events were detected in 7 players (9.6%), either in the SERPINA_A10, FactorV, FactorXII, or FactorXIII genes.
ConclusionDVT prevalence in professional soccer players is higher than expected for the same age segment, and highlights how genetic predisposition towards thromboembolic processes and sport-associated environmental risk factors work in tandem in the DVT appearance.
Venous thromboembolic disease (VTED) refers to a number of pathologies among the most important of which are deep vein thrombosis (DVT), pulmonary thromboembolism (PTE), chronic pulmonary thromboembolic hypertension, and post-thrombotic syndrome. DVT refers to the presence of a clot within a vein, accompanied by a variable inflammatory response. A PTE occurs when a clot becomes embolized in the pulmonary arterial system.
The transitory modifications of haemostasis in relation to exercise are of particular interest in sports medicine.1–5 Recent reviews and guidelines6–10 highlight that athletes may experience pro-thrombotic conditions as the result of exercise and of exposure to particular risk factors, such as trauma in vascular areas, immobilization due to injury, dehydration (which can lead to haemoconcentration and polycythaemia [also influenced by doping]11) hypoxia, and long-distance journeys during which mobility is reduced.12 All these risk factors can strongly increase the risk of a thromboembolic episode in persons with a genetic background associated with hypercoagulabilty.13
After receiving decoagulation therapy, athletes who suffer a DVT can only return to training some 6-8 weeks later, and to competition three months later. This downtime is associated with a loss of sporting condition and may incur economic losses for both the athlete and his or her club. The risk of recurrence also needs to be taken into account (especially if the patient has a predisposing genetic background) and how this might be important should the athlete become obese, develop cancer or become affected by some other clinical risk factor.7
Despite the growing number of cases of DVT reported in athletes, the prevalence of this problem has not been properly established. Such knowledge could have an impact on the diagnosis, treatment and prevention of thrombosis among athletes. The aim of the present work was to determine the prevalence of DVT in professional soccer players of the Spanish first and second divisions during the then-underway 2015–16 season, and for the previous 10 seasons (since 2005–6), and to determine the environmental and genetic risk factors associated with each recorded event.
Materials and methodsCollection of data on deep vein thrombosis eventsA questionnaire (Annex 1) was designed, based on the concepts enshrined in the Clinical Guidelines on Thromboembolism in Sport,1 consisting of 23 questions in five sections reflecting: 1) subject characteristics, 2) the suffering of a DVT event, 3) exposure to risk factors before a DVT, 4) how a diagnosis was made and the therapy provided, and 5) the duration of the time away from sport, and any recurrence.
The Asociación Española de Médicos de Fútbol (AEMEF; The Spanish Association of Football Physicians) sent the questionnaire to the medical services of the first (n = 20) and second (n = 22) division clubs taking part in the Spanish Football League (La Liga), and contacted them directly to seek their collaboration. Those services that did not respond were contacted again one month later, and again at the end of the 2015–2016 season in a last attempt to secure their enrolment.
The medical service teams of each enrolled club examined the records for the male first team players and completed the questionnaires. The apparent total number of players for whom information was available over the study period was 4962. However, players transfer between teams; once their repeated information was removed, the final total of players for whom information was available (for any length of time during the study period) was 3323 from 33 clubs.
Genetic predisposition to VTEDAll subjects who suffered a DVT (n=4), plus 73 others who did not, were subjected to Gen InCode genetic testing to identify the following variants: 1) rs6025 (the Factor V Leiden mutation) in the gene that codes for Factor V of the coagulation pathway; 2) rs1799963 in the gene coding for Factor II; 3) rs1801020 in the gene coding for Factor XII; 4) rs5985 in the gene coding for Factor XIII; 5) rs121909548 in the gene coding for SERPINC1; 6) rs2232698 in the gene coding for SERPIN A10; and 7) the variants that identify belonging to blood group A1 (rs8176719, rs7853989, rs8176743, rs8176750).13 All these genetic variants have functional effects on coagulation with the exception of the blood group A1-determining variants, all have loss or gain of function effects.13 Genotyping was performed on the DNA extracted from 400 µl blood samples in EDTA using a Maxwell® 16 IVD device. This instrument automatically purifies the nucleic acids of 16 samples per run. Genotyping was performed using TaqMan probes and the EP1 Fluidigm platform, an efficient, allele-discriminating system.
Ethics statementThis study was approved by the Comité de Estudios de Investigación Clínica de la Administración Deportiva de la Generalitat de Cataluña (9th December 2014).
ResultsBy the end of the 2015–2016 season the medical services of 18/20 (90%) first division clubs and 15/22 (68%) second division clubs had enrolled in the study. A single DVT event was recorded in the 2015–16 season. In the preceding 10 years, three events were identified (Tables 1–3). All the recorded events were associated with an official match. Two occurred in players during away games – one that required a >6 h flight home during which hydration was not well maintained, and one that required a >6 h return coach journey. Neither journey allowed for much mobility. Before travelling, the affected areas were massaged; the player who travelled home by coach also received cold and hot water baths. Two of these four DVTs were originally diagnosed as a contusion in the calf or gastrocnemius muscle “tennis leg”.14 A final diagnosis was reached in all four cases by examining the player's medical history and ultrasound examination of the venous trunks. In one case further evidence was provided by D-dimer determination and magnetic resonance imaging.15 All clots were found in the distal trunks: two in the fibula vein area, one in the sural vein area, and one in the popliteal region. The latter was associated with a contusion suffered during the game (the event recorded in the 2015–2016 season). The latter player was treated with new oral anticoagulants (NOACS), while the other three received heparin and dicumourol-derived drugs. Follow-up until return to competition was 6 months for all four affected players. No recurrence of the problem was recorded for any player. Given the total number of players whose information was available for any length of time during the study period (n = 3323), and the recording of four cases of DVT, the prevalence for this thromboembolic event is 1.2/1000 players.
Patient characteristics, clinical diagnosis and initial treatment provided.
∅ ≈ Unknown but possible. Diff.D differential diagnosis. T: training. C: competition. Physio: physiotherapy involving hot and cold water baths and/or massage.
Diagnostic methods used, treatment and estimated healing time.
HC: Clinical history, Echo: ultrasound, Dim: D-dimer, RMNi: Magnetic Resonance Imaging, NOACS new oral anticoagulants, LMWH low molecular weight heparin, Dic: dicumourol-derived agents.
Genetic predisposition towards deep vein thrombosis in the four affected players.
All.: allele; M.F.All: most frequent allele
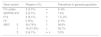
Table 5 shows the genetic background of the four players who suffered a DVT. All were carriers of the A1 risk allele at the ABO locus, and homozygous for the risk factor allele of Factor XIII. One of these players (player 3 in Table 3) was also heterozygous for the risk factor allele of Factor XII. A further 73 players from one first division and two second division clubs were also tested. None of these suffered a DVT nor did they report such an event having occurred in any first degree relative. Two were heterozygous for the SERPIN A10 gene rs2232698 variant, three were homozygous for the risk factor variant of the gene for Factor XII, and two were homozygous for the Factor V Leiden variant.
Genetic predisposition to deep vein thrombosis in the 73 players who suffered no thrombotic event.
| Gene variant | Players n (%) | Prevalence in general population | ||
|---|---|---|---|---|
| FV Leiden | 2 (2.7%) | ≈ | 2–3% | |
| SERPIN A10 | 2 (2.7%) | ↑ | 1.6% | |
| F12 | 3 (4.1%) | ↑ | 1.5–2% | |
| F2 | 0 (0%) | ↓ | 2–3% | |
| ABO* | 0 | 54 (74%) | ↑ | 56.6% |
| 1 | 16 (21,9%) | ↓ | 38.1% | |
| 2 | 3 (4.1%) | ≈ ↓ | 5.3% | |
The prevalence of VTED recorded for the present players – in this case always DVT- was 1.2 per 1000, the same as for all first VTED events in the general population.16 However, for the 18–35 years age group in the general population the expected figure is just 1/10,000 people17 – much lower than that recorded for the players (aged 26.4 ± 4.2 years). It is possible that the prevalence reported here could actually be higher given the possibility of unrecorded asymptomatic or undiagnosed events.1819 While physical activity and structured exercise are recommended for the prevention of cardiovascular disease, training exposes athletes to thrombogenic risk factors such as heat stress, dehydration, haemoconcentration, blood vessel lesions, and inflammation; long journeys to matches may also involve immobilisation.1–7 This may explain the greater prevalence of events detected among the players.
It may be that the prevalence of DVT among athletes of other sporting disciplines is also high, especially if they are subject to the same environmental prothrombotic factors,20 in particular physical contact. DVTs have recently been reported suffered by basketball players9 and marathon and mountain ultra marathon runners21 (many competitors in these latter two sports are older and may no longer have the most adequate venous health). In addition, a recent study7 reported 47 cases of DVT in athletes after completing intense aerobic exercise. Half of those affected had been through a recent prolonged period of inactivity or were genetically predisposed to thromboembolic disease (usually undiagnosed). The time lag between the first symptoms and a confirmed diagnosis was 56.3 ± 118.7 days (25 cases [53.2%] were initially incorrectly diagnosed). Importantly, seven months elapsed before these athletes could begin competing again.
Recent reviews coincide in that DVT in athletes is often diagnosed incorrectly or late,6,21 often because athletes themselves underestimate the seriousness of their lesions.15 Late diagnosis increases the potential seriousness of the problem; anticoagulation therapy for DVT and pulmonary embolism is required immediately.
In the present players who suffered a DVT, the lesion was always distal. Fortunately, distal DVT is more unlikely to cause a PE than a proximal DVT.9 However, 20–30% of distal DVTs become proximal if they are not treated, and proximal clots are much more likely to cause a PTE,22 over 50%. It is therefore important to reach a diagnosis rapidly and begin treatment quickly.10 At the time of writing, none of the four affected players has suffered any further thrombotic event.
It is important to note that the 73 teammates who suffered no DVT were subject to the same kind of sports-environment thromboembolic risks as the four players who did suffer a DVT. Seven of these 73 (9.6%) also had a genetic predisposition to such problems, but since they suffered no DVT It is possible that exercise per se decreases the likelihood of thromboembolic events despite predisposition, or that the four players who experienced thromboembolic events were exposed to some other unknown risk factor, or to several that act synergistically.
ConclusionIn summary, the present results show that the incidence of DVT in Spanish League first and second division soccer players is higher than that seen for the same age group in the general population. They also highlight how genetic background and the environmental factors particular to sport work in tandem to increase the risk of DVT. In addition, they suggest that preventive measures need to be developed based on players' medical histories, their family history of haemostasis problems, adequate hydration, mobilisation, early diagnosis, and genetic studies in those whose medical/family background make this advisable. Finally, it is of the utmost importance that sports doctors and players alike be aware of the risks of suffering a DVT, and to take precautionary and corrective action as required.
The authors would like to thank the Spanish Football Medical Association AEMEF, in particular to Dr. Paco Angulo, president of the Association at the time of this study, for his involvement, support and facilities to address all our concerns. Thanks also to the medical doctors of the clubs of the First and Second Spanish Division, who were seriously involved from the very beginning, their work has been fundamental to the achievement of this study. Special thanks are due to Lluis Til, Ricard Pruna and Javier Ismael Yanguas of FC Barcelona's Medical Service, for their wise comments and support throughout all the process.
Authors contributions:
Franchek Drobnic (FD), Jose Manuel Gonzalez de Suso (JMGS), Antonio Turmo (AT), Mindaugas Gudelis (MG), Xavier Valle (XV), Xavier Peirau (XP), Juan Carlos Souto (JCS), José Román Escudero (JRE), José Manuel Soria (JMS).
FD and JMS participated in the development of the idea, design of the study, monitoring, data collection, logistics, elaboration of the discussion, statistical evaluation, elaboration of the final document. JMGS, AT, MG, XV, XP, JCS, JRE contributed in monitoring of the study, data collection, logistics, elaboration of the discussion and the final document.
Competing interests:
The authors declare that they have no competing interests.
None of the authors has any commercial or competitive interest in the development or in relation to the final results obtained from this research project.