There is a high incidence of non-contact anterior cruciate ligament (ACL) injury in team sports, especially among adolescent females. This injury is associated with an increased risk of developing osteoarthritis later in life and a decrease in lifetime physical activity. Traditionally, return-to-sport (RTS) programs following ACL injury have focused on restoring the athlete's general health and tissue healing. We will propose a framework that views RTS as a two-part process: first, recovery of general health after ACL reconstruction (ACL-R) (rehabilitation) and then return to competition (RTC) after ACL-R, all of which occurs on a continuum. The objective of Part I is to stablish the foundation to propose an evidence- and experience-based guide on RTS following ACL reconstruction in athletes participating in team sports, specifically for later phases. First, we describe the causes of and risk factors associated with ACL injury. Next, we describe the specific characteristics of team sports that predispose athletes to ACL injury. Finally, we present a progressive framework to successfully return athletes to a pre-injury level of competition that also minimizes risk of reinjury. In Part II we will focus on how to put the proposed framework into practice when return team sport athletes to play following ACL-R.
The perceived severity of anterior cruciate ligament (ACL) injury makes it highly feared by athletes. Not only does ACL injury result in a long period of absence from sport,1 but it has also been associated with an increased risk of developing osteoarthritis later in life and a decrease in lifetime physical activity. 2
Non-contact ACL injury is related to alterations in movement patterns during dynamic scenarios (e.g. increased knee valgus during a change of direction). These alterations are associated with deficits in neuromuscular control (e.g. hamstring weakness). Neuromuscular training interventions have been developed to improve deficits in neuromuscular control and to reduce non-contact ACL injury risk.3,4 Despite the existence of these training programs, the incidence of ACL injury remains relatively high, especially among female athletes whose risk of injury is 2–10 times that of male athletes.5
Typically, ACL injury requires athletes to undergo reconstruction (ACL-R) to return-to-sport (RTS).6 Following ACL-R, athletes face a long process of rehabilitation and conditioning before they can safely return to competition (RTC) at a pre-injury level. Ardern et al. (2010) observed that only about a third of team athletes return to sport at or above their pre-injury level of competition within a year of injury 7. The combined risk of ACL reinjury to the same ACL or injury to the contralateral ACL is 6–32%. 5 The risk of ipsilateral/contralateral ACL injury is greatest in youth athletes attempting to return to high-level competition, which should be of particular concern to practitioners working with this population.8 In fact, research suggests that a quarter of youth athletes who have sustained an ACL injury will experience reinjury.9 To avoid the serious social and economic consequences that may result from reinjury, it is imperative that rehabilitation programs be sport-specific. Traditionally, clinical practice guidelines have focused on the early phase of rehabilitation. They tend to generalize the recommendations relating to RTC.10 To optimize RTC, the focus should be expanded to include an emphasis on preparing the athlete for successful mastery of team sport-specific demands.
Currently, no consensus on the optimal training program to return athletes to sport following ACL-R exists. The objective of this study (Parts I and II) is to address the current deficiency of the RTS literature by providing an evidence- and experience-based guide for practitioners to create successful RTC training interventions in team sport athletes following ACL-R. A literary search of Sport Discus, Medline, and Google Scholar was made until May 2020. The main search algorithm used were (ACL) AND (return to play OR return to sport OR rehabilitation). The reference lists of any articles pertaining to ACL and sports team were scanned for further studies that were relevant to this study. In this first part, we describe the etiology of ACL injury. We will also discuss the specific characteristics of team sports that leave these athletes susceptible to ACL injury. Finally, we will propose a progressive framework to RTC that is intended to maximize the athlete's performance while minimizing risk of reinjury. In the second part, we will provide a more extensive description of this framework to return athletes following ACL-R to team sports training and competition.
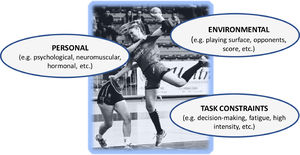
Injury etiologyMost sports injuries are multifactorial and result from complex interactions. This is especially true in team sports.11,12 Normally, athletes repeatedly engage in high-risk situations without sustaining injuries. However, when certain conditions are met, including an interaction of personal factors (e.g. psychological, neuromuscular, anatomical, hormonal, etc.), the environment (e.g. playing surface, opponents, score, etc.) and task constrains (e.g. decision-making, fatigue, and intensity), the same situations that had been successfully navigated previously can result in ACL injury (Fig. 1). To successfully implement the RTC process following ACL injury, it is essential to understand injury etiology. This includes having a firm understanding of both injury mechanisms and the risk factors for injury, especially those that can be modified.
Injury mechanismsMechanisms of ACL injury vary by individual, by sport, and by sport-specific situations. Though each ACL injury is unique, many of the injuries sustained during team sports have common elements. A majority of ACL injuries are non-contact injuries, which account for 37.5–85% 13,14 of all ACL injuries. In addition, the most common non-contact mechanisms of injury during sport are a combination of deceleration, change of direction and/or jump landing actions. Video analysis of non-contact ACL injuries has shown that these high-risk actions are accompanied by: 1) dynamic knee valgus, 2) near-full knee extension, 3) total weight supported by the injured leg and sole of the foot fixed in the ground, and 4) lateral trunk inclination.15 All of these mechanisms trigger anterior tibial translation, which can result in ACL injury 16. While the mechanisms described here occur in all athletes, they occur more severely in female athletes 16. Fatigue and decision-making, which common elements in team sports, exacerbate these high-risk movements leaving athletes susceptible to ACL injury.17
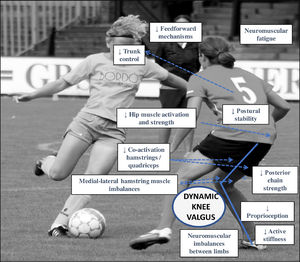
Risk factorsAs previously mentioned, analysis of ACL injury risk factors is essential to the success of any RTC plan. There are two generic classifications for ACL injury risk factors in sport: intrinsic and extrinsic.18 Extrinsic risk factors include, among others, unstable playing surfaces (e.g. resin or water on the court) or adverse environmental conditions (e.g. rain) during training or competition. Intrinsic risk factors include stage of maturation, sex (females at greater risk than males), higher body fat and certain anatomical characteristics of the knee joint and ACL. Additionally, factors related to the physical capabilities of the athlete are considered intrinsic, such as poor hamstring strength and poor proprioception.19 Another important system further classifies non-contact ACL risk factors into four categories: environmental, anatomical, hormonal and neuromuscular 19. The latter two categories are believed to be modifiable through training.20Fig. 2 demonstrates the relationship between the most common ACL injury mechanism (dynamic valgus) and its associated neuromuscular deficits. In this case, poor neuromuscular control is associated with altered movement patterns that lead to non-contact ACL injury.
Current best evidence shows the modifiable neuromuscular and biomechanical risk factors that contribute most to non-contact ACL injury and reinjury are1,21-24: 1) deficits in neuromuscular control of the lower limb resulting in reliance on frontal plane over sagittal plane strategies (dynamic valgus or ligament dominance), 2) dominant use of the quadriceps muscles over the hamstring muscle to stabilize the knee (quadriceps dominance), 3) significant inter-limb asymmetries in strength, coordination and proprioception (leg dominance), 4) decreased core stability (core dysfunction), 5) neuromuscular fatigue and, 6) diminished feedforward mechanism. Fortunately, there is an abundance of literature that details how to modify risk factors through targeted neuromuscular training, especially in those at greatest risk of ACL injury (pubertal females).3,4,25Table 1 lists each modifiable risk factor and some neuromuscular training strategies to correct them.
Relationship between the main modifiable risk factors for non-contact ACL injury and their associated corrective neuromuscular training strategies.
In addition to injury etiology, to return athletes to sport it's important to understand the characteristics of team sports that lead to ACL injury, such as the physical demands and the skills needed to successfully compete.
Performance in team sports depends not only on physical fitness (e.g. ability to repeat high intensity actions) and sport-specific skill/technique, but also on cognition (decision-making), creativity, and emotional-volitional and socio-affective elements.26 Team sports are also called “situational” sports because the interactions among the environment, teammates, direct or indirect opposition and continuous decision-making lead to a high degree of variability in each session of training or competition. Movement patterns in team sports change constantly.27 Consequently, athletes must possess high levels of fitness, technique and tactical skill to successfully perform in the unpredictable and hyper-complex scenarios that characterize team sports. Due to the nature of team sports, the training principle of variability is key when returning athletes to sport following ACL-R. Athletes must re-learn how to compete in the hyper-complex environment.
Physically, team sport athletes must be able to repeat and combine high-intensity activities (e.g. accelerations, decelerations, sprints, changes of direction, jumps and technical skills) in short intervals for the duration of 40–90 min games, depending on the sport.27 Many sports place demands on both aerobic and anaerobic systems in combination with low- and high-intensity activities.28 Sport-specific demands require significant energy expenditure, causing athletes to become physically, metabolically and mentally fatigued. In small field sports, such as basketball and handball, athletes usually cover total distances between 4 and 6 km29,30 over the course of a game, though the distance varies by position. In large field sports, such as soccer and field hockey, athletes usually cover total distances between 8 and 12 km31,32 This difference in small and large field sports highlights the importance of understanding the general physical requirements of the team sport. It's also important to understand the demands of the position, the level of play, and the contributions of sex to each of these.
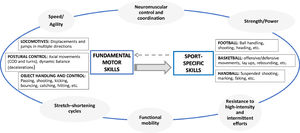
Despite the fact that each team sport requires its own specific skills (e.g. shooting on goal in soccer, dribbling in basketball, or defensive moves in handball), most teams sports share fundamental motor skills (FMS) (e.g. throws, changes of direction, displacements or jumps). For this reason, during the RTC process it is essential to start with re-learning of FMS, beginning with the least demanding and progressing to those that compromise the stability of the knee the most (e.g. decelerations, changes of direction, and jumps). The skills should progress in a personalized way that builds toward allowing the athlete to re-learn sport specific skills (SSS), and culminates in the incorporation of those SSS, especially high-risk skills, in a hyper-complex environment. In addition to progression in skill, the RTC plan should progress in terms of physical demand. For example, in the early phases of RTC the resistance training emphasis is on strength. In the final phases of RTC the resistance training emphasis is on power-endurance, which is a necessary for success in team sport competition.
Planning the return to competition at optimal performanceIn rehabilitation, it is customary to follow injury treatment protocols. Our proposed progressive framework departs somewhat from the traditional protocols, or recipes, for RTC. Each injury is unique, and recovery depends on many factors, including individual athlete characteristics, injury history, sport, injury etiology, surgery/graft type and concomitant injury. Each RTC plan must be tailored to the individual by using the different domains described here to optimally return athletes to pre-injury levels of competition. Our progressive approach will not focus on time; rather, we will describe criteria, or “approaching levels”, that can be used to progress rehabilitation and RTC plans in task complexity and specificity.33 Currently, there is no consensus on the optimal time for RCT following ACL-R. Research suggests this can be done from 4 to 6 months (2) to 6–12 months5 after ACL-R. Other research recommends delaying return to top-level competition for two years after ACL-R.34,35
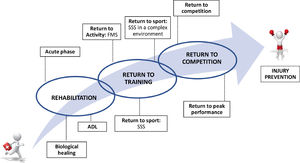
While we agree with the overall concept of the last published consensus on RTC after ACL-R, which attempts to frame the RTS process as a continuum without phases, we will differentiate between the processes of returning to training and of returning to competition (Fig. 3) 10. Rehabilitation focuses on healing injured tissues and on restoring the athlete's general health.36 In contrast, RTC focuses on maximizing conditioning and performance, which are necessary to return athletes to competition, and minimizing risk of injury and reinjury. While complete recovery of injured structures is important, this alone is not sufficient to return athletes to sport. The first phase of RTC involves training with the team. The goals are to improve the athlete's conditioning, coordination, cognition, and emotional state. From there, the progressions should be tailored to the athlete and build to the ultimate goal of preparing the them to withstand high loads in hyper-complex situations while minimizing injury risk. Interdisciplinary work is an important part of the rehabilitation/RTC process. Different professionals from both the technical and medical teams must work together to support the athlete's successful reintegration.37
In summary, RTS has two objectives. The first objective is to prevent ACL reinjury by reducing modifiable risk factors and improving the physical condition (improve health). The second objective is to prepare the athlete to compete at the highest levels of exertion in a hyper-complex environment (maximize performance).
ACL post-injury RTC frameworkAlthough this section is described in greater detail in Part II, we aim to present a flexible approach to training following ACL-R to successfully return team athletes to sport. To create this progressive framework, we adapted Paco Seirul·lo's “structured training” planning model (Fig. 4), which is widely used in team sports.33 This model provides a useful framework for structuring the RTC process following ACL-R. It is based on the idea that to optimize specific motor skills (sport-specific movements), you must first develop the fundamental or general motor skills (areas) that support them. For example, to successfully execute a lay-up in basketball (sport-specific movement), an athlete must first master the general motor skills that comprise it – running, jumping and throwing (Table 2 and video 1).
Framework for return to competition following ACL-R in team sports. The framework proposes an integrated and flexible RTC approach that combines the work of skills (fundamental and sport-specific) with physical capabilities (Strength/power, speed/agility, neuromuscular control and coordination, stretch-shortening cycles, functional mobility and resistance to fatigue). In addition, it also integrates the cognitive, perceptual and emotional structures (systems), performance characteristics in team sports. (RTC: return to competition; ACL-R: anterior cruciate ligament reconstruction; COD: change of direction).
Return to sport proposal centered on layup in basketball and based on “approaching levels”. The table shows examples tasks to improve strength and neuromuscular control during a lay-up with contact in basketball using “approaching levels”. The table shows a progression in specificity of tasks emphasizing three basic areas or fundamental motor skills (Linear displacement, single-leg jump and fight) for specific development of a lay-up with contact in basketball (Specific motor skill) (Video 1).
The progressive framework to RTC following ACL-R presented here combines the simultaneous development of skills (fundamental and specific) and physical capabilities (strength/power, speed/agility, neuromuscular control and coordination, stretch-shortening cycles, functional mobility and resistance to fatigue) (Fig. 4) 38. The focus should not be limited to “conditional” and “coordinative structures” (systems); instead, the focus should be expanded to include integrate “cognitive”, “perceptual” and “emotional structures” (systems). Following the basic training principles of progression and individualization, RTC should begin with the reinforcement of FMS (e.g. vertical jump) in conjunction with general physical capabilities (e.g. strength-endurance). It should then progress toward the acquisition of SSS (e.g. soccer shooting in a game context) in conjunction with sport-specific physical capabilities (e.g. ability to repeat high-intensity actions), which simulates the complexity of team sports (Fig. 4). Components of rehabilitation and RTC should not be considered in isolation; rather, they should be integrated with one another in a flexible way through progression without losing sight of the athlete's injury experience (e.g. pain, edema, etc.).
In order to optimally plan RTC following the aforementioned team sport methodology, training can be structured at different “levels of approach” to sports movement,36,37 (Table 2 and Video 1). Training can be generic, general, directed, special or competitive and ranges from low to high specificity. To identify and classify the tasks, six levels of approach were established (0-, 0+, I-IV) that progress in complexity according to their degree of similarity to sports competition. In the case of RTC, in earlier stages, general orientation tasks are used as a priority (0-, 0+, I) and progress is made towards a more directed nature (II and III). As the injured athlete tolerates the loads and gets closer to returning to competition, they move towards more specific and demanding tasks, called special (IV) and competitive (V). In other words, the first levels of approach are associated with “coadjuvant training”,40 or tasks that aim to: 1) improve the well-being and health of the athlete, and 2) allow the athlete to tolerate and successfully develop the specific tasks essential to sport competition. The final levels of approaching are associated with training that prepares the athlete for competition. These tasks must be carried out in authentic game environments 39Table 2 and Video 1 shows examples of tasks at each level of approach for the retraining of a contact lay-up in basketball, a situation that puts athletes at high risk of sustaining ACL injury.
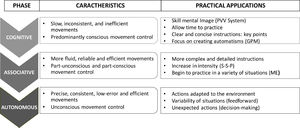
Finally, it is important to apply the principles of motor learning and practice constraints because they are key to facilitating and optimizing the relearning of basic and specific skills after ACL-R.41 The practitioner's instructions and feedback are necessary components to maximizing motivation and attitude during training. Additionally, emphasis should be placed on conditions that facilitate learning (e.g. variability or randomization of tasks) and those conditions should be appropriate for the level of the learner 42Fig. 5 demonstrates practical applications at each phase of Fitt's and Posner's recovery (cognitive, associative or autonomous) to progress athletes following injury.43 For example, in the first phase of relearning a skill, it is important to automate skills in controlled situations. As the athlete is near to competition, tasks can be progressed under conditions of fatigue with disturbances and/or with complex decision-making.
Practical application in return-to-sport according to motor learning phases (Fitts & Posner, 1967). The figure divides motor learning into three phases of progressive difficulty (cognitive → associative → autonomous). PVV: Propioceptive, visual and vestibular; GPM: General pattern of movement; S-S-P: Strengh, speed and power; ME: motor scheme.
To successfully return athletes to sport and competition following ACL-R, the first step is to understand factors that contribute to ACL injury. These factors include the mechanism of injury and risk factors for injury, especially those that are modifiable. Modifiable risk factors that are related to the athlete's condition, such as physical fitness, and neuromuscular and biomechanical imbalances that lead to the injury, are particularly important to consider. Integrated neuromuscular training plays a special role in RTC following ACL injury because it works to improve imbalances that predispose athletes to injury. In conclusion, recovery from ACL-R and improving ligamentous integrity alone are not sufficient to return team athletes to competition. It is essential to also prepare athletes to withstand the demands of a chaotic and unpredictable team sport environment.